Case for iPhone – IBOOLO
People May Ask
The protuberances vary in size, measuring from a minute 1 or 2 millimeters up to several millimeters in diameter. Their hue often matches the complexion of one's skin, albeit they might also exhibit a subtle whiteness or a touch of yellowness. Notably, these bumps are typically painless and do not elicit itching sensations. However, it's worth noting that they might bleed if accidentally knocked or shaved over.
Upon the emergence of sebaceous gland hyperplasia, it persists without spontaneous resolution. This is attributed to the fact that a lesion resulting from sebaceous gland hyperplasia comprises a cluster of sebaceous gland cells, commonly referred to as sebocytes.
When seeking an initial non-prescription remedy, opt for creams fortified with retinol or vitamin A as the primary active constituent. Retinol effectively safeguards against the clogging of pores due to excessive oil build-up.
The pinhole technique entails the utilization of an ultra-pulse carbon dioxide (CO2) laser to meticulously create an array of minute perforations, extending from the superficial epidermis layer down into the deeper realms of the dermis.
Options for treatment encompass facial exfoliation, laser-based interventions, cold therapy, electric cauterization, photodynamic treatment methodologies, prescription of antiandrogenic medications, as well as surgical procedures. The expenses associated with each of these treatment alternatives vary and will be thoroughly addressed with you by your consulting dermatologist.
The phenomenon arises as a result of the augmentation of the sebaceous glands, also known as oil glands. While it's typical to encounter one or two occurrences, there are individuals who may possess a dozen or even more due to their genetic predisposition. On the skin's surface, this manifests as a subtle, yellowish protrusion, typically measuring between 2 and 5 millimeters in diameter. Upon closer inspection, a minute central opening can frequently be discerned.
What are the underlying factors that contribute to the development of sebaceous hyperplasia? Hormonal fluctuations are among the primary culprits, instigating this condition. For instance, individuals who were designated male at birth (AMAB) experience a decline in androgen levels as they grow older. This decrease prompts a reduced turnover rate of sebocytes, subsequently encouraging the proliferation of additional sebocytes within the sebaceous glands.
Distinct from sebaceous hyperplasia, a sebaceous adenoma observed in this microscopic view comprises sebaceous lobules characterized by a 2-cell variety of sebocytes, unlike the single-cell pattern seen in the former condition.
Sebaceous hyperplasia manifests in the form of solitary or multiple papules, ranging from 1 to 3 millimeters, with a yellowish hue, predominantly on the facial area, especially the forehead, of adult individuals. Frequently, these papules possess a central pore, signifying the follicular infundibular opening, and are accompanied by superficial telangiectasia. In clinical settings, these lesions may be erroneously identified as BCC.
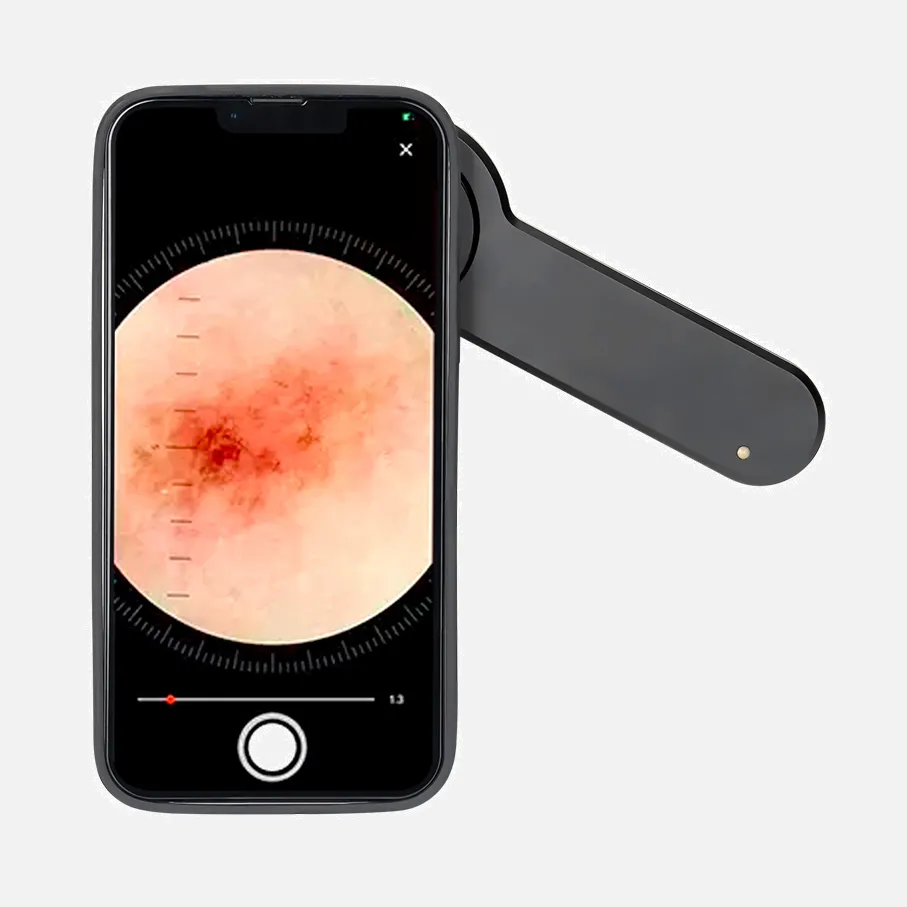
The diagnosis of sebaceous hyperplasia is typically established through clinical assessment, often augmented by dermoscopic evaluation. In scenarios where differentiation from basal cell carcinoma is required, a biopsy may be deemed suitable. Upon histopathological examination of sebaceous hyperplasia lesions, it is evident that the glands exhibit enlargement yet maintain their standard morphological features.