Case for iPhone – IBOOLO
People May Ask
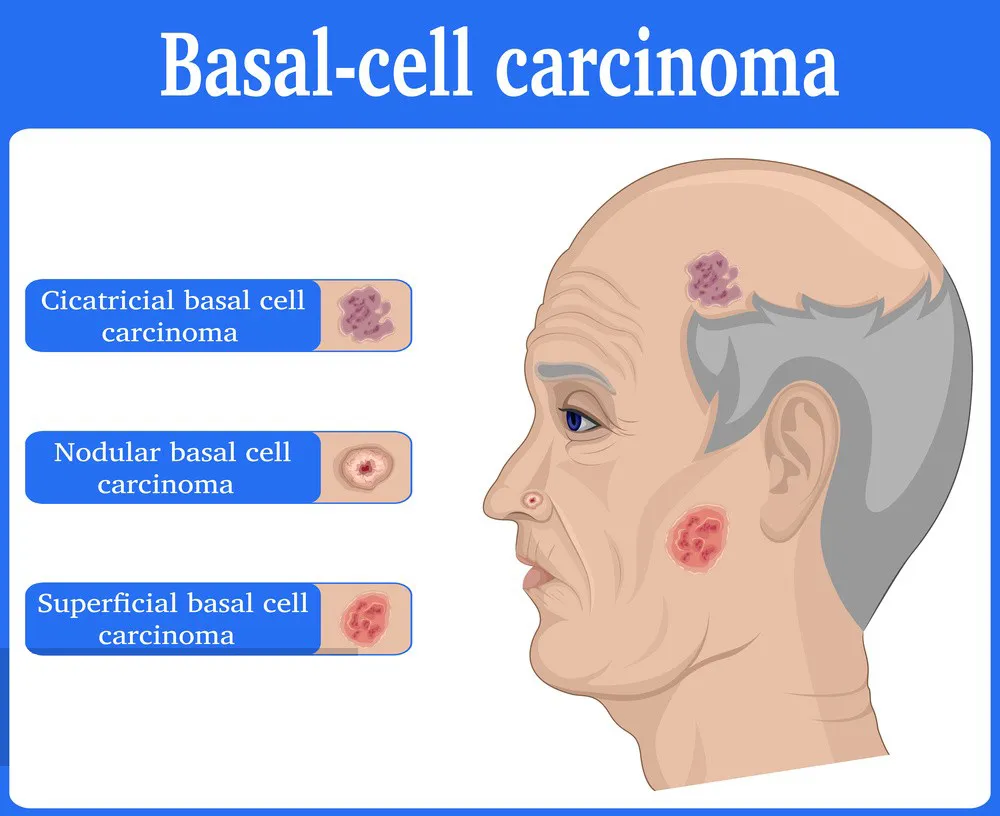
The distinctive hallmark of BCC lies in its waxy, pinkish, and pearlescent visual aspect. Typically, these abnormal growths encompass conspicuous subepidermal blood vessels, also known as telangiectasia, alongside the presence of ulceration. It is crucial to underscore that BCCs are predominantly observed on skin areas with hair follicles, with a particular predilection for the facial region.
The term "Bcc" utilized within an electronic communication signifies a blind carbon copy. By Bcc'ing a recipient, one disseminates a duplicate of the email message while ensuring their email address remains concealed from the remaining recipients. Furthermore, this action disables the capability for a "reply-all" response.
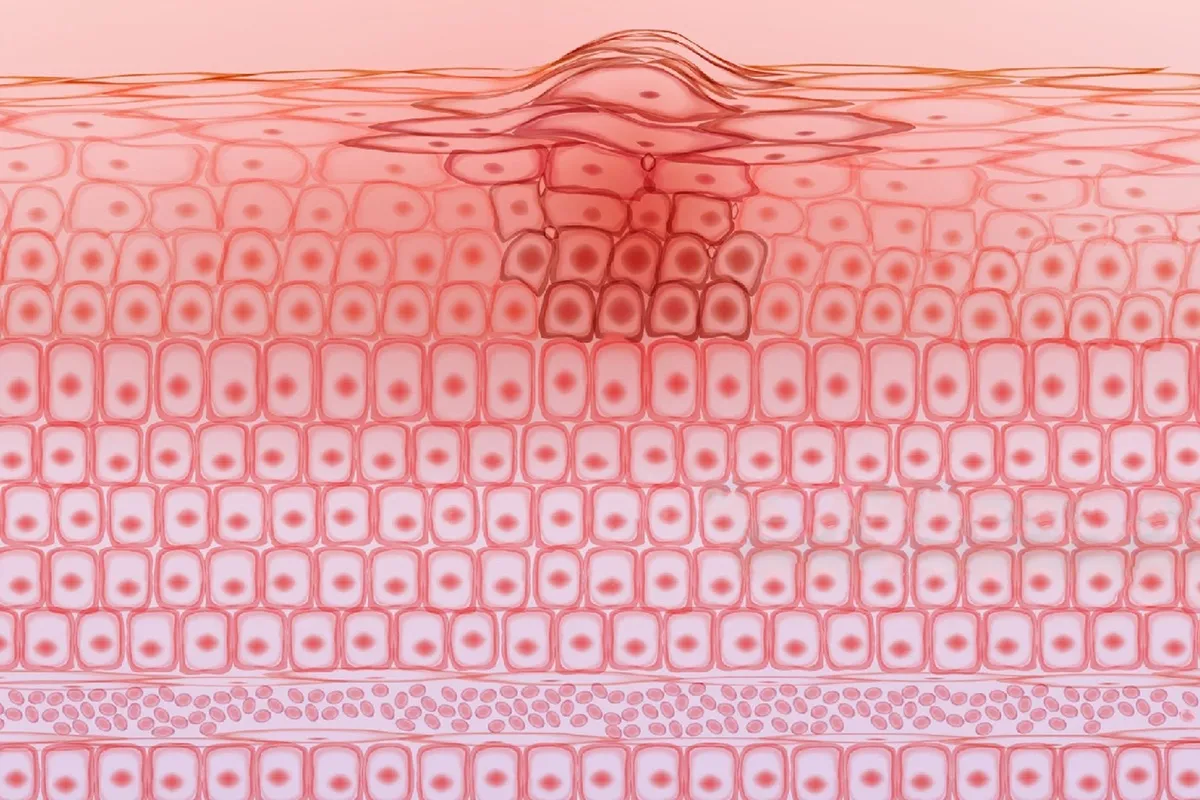
The histological structure of basal cell carcinoma exhibits a characteristic arrangement, wherein the basaloid epithelium assumes a palisaded pattern, accompanied by the emergence of a cleft that originates from the adjacent stromal tissue of the tumor (depicted in Figure 2). Within this central region, the nuclei exhibit a congested appearance, interspersed with discernible mitotic figures and necrotic remnants (visible in Figure 3).
Prompt identification of basal cell carcinoma correlates positively with improved survival prospects for patients. Current therapeutic modalities aimed at treating this condition boast a recurrence-free cure rate ranging from 85 to 95 percent.
The underlying factor contributing to basal cell carcinoma (BCC), the prevalent form of skin malignancy, is widely acknowledged. The majority of individuals experience its onset due to severe harm inflicted upon their skin by ultraviolet (UV) radiation emanating from two primary sources: direct exposure to sunlight and the utilization of indoor tanning devices, inclusive of tanning beds and sunlamps.
An area of skin will develop a protective layer known as a scab. The duration for the wound to fully recover can range from 3 to 6 weeks, contingent upon the extent of the treated region. Adequate wound management can contribute to the gradual diminishing of the scar over time.
Basal cell carcinoma (BCC) infrequently progresses to a late stage, rendering the administration of systemic chemotherapy as an uncommon treatment modality for such malignancies. Instead, advanced basal cell cancers are more inclined to be managed through targeted therapy or immunotherapy.
If not properly addressed, it has the potential to deteriorate into bone, cartilage, and the skin surrounding it. This deterioration can give rise to disfigurement and hinder normal functioning, especially when it affects the face, nose, or ears. Lack of Prompt Diagnosis: Disregarding BCC might contribute to a delayed recognition of the condition.
Less than 1 percent of basal cell carcinomas, the prevalent type of cancer encountered in the United States, propagate (metastasize) beyond their initial tumor site. This particular carcinoma manifests as an unusual skin protrusion, lump, or lesion that tends to develop gradually and can be effectively managed through surgical intervention.
Surgical excision for biopsy
The most suitable therapeutic approach for nodular, infiltrative, and morphoeic forms of BCC necessitates the inclusion of a 3 to 5 millimeter border of healthy skin encompassing the tumor. In cases of extensive lesions, a flap reconstruction or skin grafting may be necessary to address the resulting defect.