Case for iPhone – IBOOLO
People May Ask
Although melasma has the potential to fade naturally over time, this particular skin discoloration can persist for extended periods, spanning years. Should you find the appearance of melasma-induced pigmentation on your skin undesirable, there are therapeutic options available that may offer assistance. Dermatological experts advise addressing melasma promptly, as early intervention is often preferred.
Melasma presents in three fundamental varieties, each tailored to a distinct therapeutic approach.
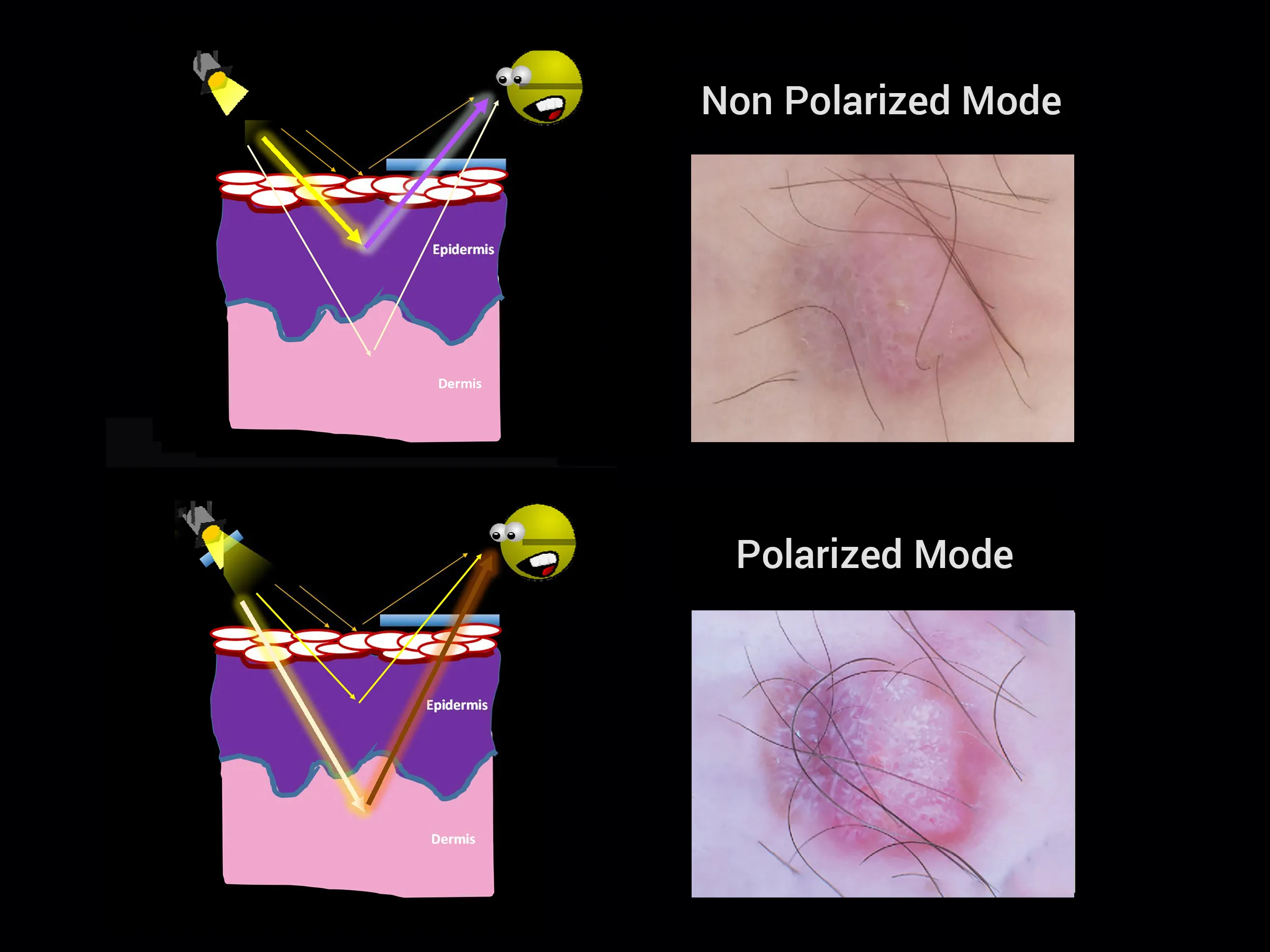
The first manifestation is Epidermal Melasma, a form that specifically targets the outermost layer of the skin. ...
Subsequently, there's Dermal Melasma, the second variant, which infiltrates the deeper layers of the skin, particularly the dermis. ...
Lastly, we have Mixed Melasma.
Consumption of vitamins such as C, E, B3, and D can aid in maintaining skin health and alleviating melasma symptoms. Nevertheless, a deficiency in these vitamins may exacerbate skin conditions or lead to additional concerns. Consequently, it is advisable to seek the guidance of a dermatologist in Pune for an assessment and to discuss appropriate vitamin supplementation for melasma treatment.
Melasma arises in regions that are frequently exposed to sunlight, manifesting as a form of secondary hyperpigmentation. This condition appears as evenly spread, hyperpigmented spots, which may either blend together or be distinct and punctate. The severity of melasma intensifies in areas subjected to prolonged and intense sunlight, notably the cheeks, the superior lip, the chin, and the forehead.
The presence of hyperpigmentation could be indicative of sun-induced damage or solar lentigines, particularly in individuals with a prolonged history of continuous sun exposure and the practice of tanning. In contrast to these, melasma typically manifests in the form of larger, broader areas of skin discoloration. Conversely, sun spots and alternative types of hyperpigmentation tend to resemble minute circular shapes or distinct focal points.
Frequently, an efficacious approach to treatment involves incorporating sunscreen protection alongside topical medications tailored for your skin, and in certain cases, a specialized procedure. When seeking treatment for melasma, it's crucial to inquire about the associated costs from your dermatological professional.
On July 24th, 2023, it was highlighted that melasma presents itself in three primary categories: the epidermal variant, the dermal type, and a blend of both, known as mixed melasma.
Upon the emergence of melasma, it tends to manifest as pigmented patches ranging in hues from tan to brown, grayish brown, or even bluish gray, resembling freckles. These occurrences are predominantly observed on specific facial regions, such as the cheeks, forehead, chin, and occasionally above the upper lip. While less prevalent, melasma can also manifest on the arms, neck, or other body parts.
What are the indicators and manifestations of melasma?
Melasma triggers discolorations and blotches that exhibit a darker hue compared to one's natural skin tone. ...
Melasma tends to emerge symmetrically on both halves of the face. ...
It has the potential to cover significant portions of the skin. ...
In some regions, melasma may be more pronounced than in others. ...
Melasma can manifest on the lateral aspects of the face.
Additional points...•
Some skin conditions that are frequently mistaken for melasma are:
Actinic and plain lichen planus.
Pigmentation caused by certain medications.
Guttate hypomelanosis, a skin condition.
Exogenous ochronosis triggered by hydroquinone.
Lentigo, also known as age spots.
Hori's nevus.
Ota's nevus.
Post-inflammatory pigmentation, a consequence of skin inflammation.