Case for iPhone – IBOOLO
People May Ask
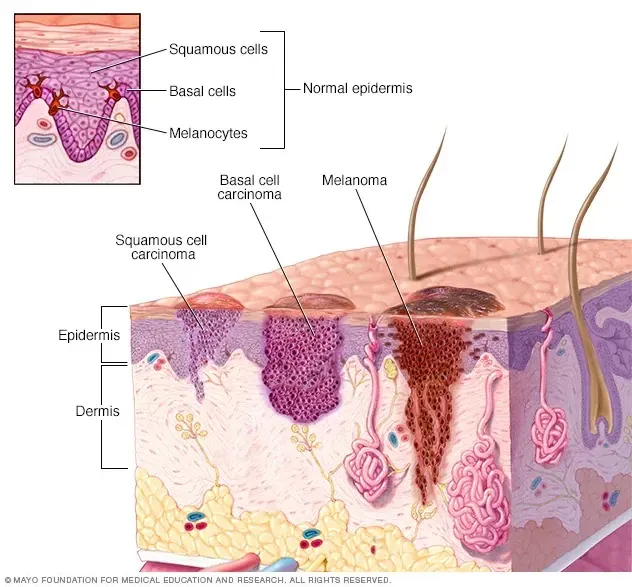
KEY FINDING: Investigators uncovered a notable escalation in the adjusted probability of being diagnosed with melanoma in situ among Caucasian males and females, with a surge from 0.17% to 2.7% for men and from 0.08% to 2% for women, spanning the period from 1975 to 2018.
As of 17th February, 2024, individuals diagnosed with stage 0 melanoma, also known as melanoma-in-situ, exhibit a 5-year relative survival rate of 97%, significantly higher than the 30% observed in patients with stage IV melanoma.
The lifespan with an undetected melanoma varies significantly, contingent upon the progression stage of the condition. The prognosis for individuals with localized melanoma boasts a 5-year survival rate of 99%, whereas for those with melanoma that has spread, the rate diminishes to 30%. January 17th, 2023.
The dermatoscopic methodology known as the Seven-Point Assessment Protocol [1] outlines essential indicators for analysis, with two major criteria assigned two points each: an unusual pigment network formation, and the presence of a blue-white veil alongside an atypical vascular arrangement. Additionally, four minor criteria are assigned one point each, including irregular streak patterns (or pseudopodia), scattered irregular dots or globules, an eccentric area of hyperpigmentation (indicative of irregular pigmentation), and discernible regression structures. Updated on Feb 9, 2023.
Certain medical professionals refer to melanoma in situ as a precursor to cancer. This form of melanoma can be successfully eradicated through surgical intervention. Nevertheless, in the absence of proper treatment, melanoma in situ has the potential to progress into a more aggressive type of cancer, known simply as melanoma.
A scarce minority inherits genetic markers predisposing to melanoma
Roughly 10 percent of melanoma cases stem from genetic variations (alterations) transmitted across familial lines. However, the vast majority of melanoma occurrences are attributed to alternative factors. Exposure to the sun, as well as artificial tanning methods such as beds and lamps, emit ultraviolet (UV) radiation, which is a well-documented contributor to skin damage.
The diagnosis of Stage 0 melanoma, also known as melanoma in situ, indicates a highly treatable condition. The chances of recurrence or metastasis are extremely low.
The majority of occurrences of Ductal Carcinoma In Situ (DCIS) are asymptomatic, lacking a discernible lump, and are primarily identified through routine mammographic screenings. In fact, a staggering 90% of DCIS instances are uncovered through these preventative mammography tests.
The prevalence of melanoma overdiagnosis has emerged as a pressing contemporary concern, particularly amidst the surging counts of in situ melanoma cases. This commentary piece delves into the phenomenon, often labeled as the "overdiagnosis pandemic" within the realm of melanoma diagnosis.1st October, 2023
The recommended therapeutic approach for melanoma at Stage 0, also known as in situ melanoma, revolves around surgical intervention. The core objective of this surgical procedure is to eradicate any residual cancerous tissue that might have been left behind following the biopsy. This method is commonly referred to as a comprehensive local excision.