Case for iPhone – IBOOLO
People May Ask
In recent times, scientists have formulated innovative therapeutic strategies for tackling advanced stage 4 melanoma. Notably, several immunotherapy approaches have yielded promising outcomes up until now. Thanks to these novel treatments, certain individuals are managing to coexist with stage 4 melanoma for extended periods. Furthermore, there is a possibility that a subset of these patients may eventually discontinue treatment and enjoy a prolonged lifespan. Date:
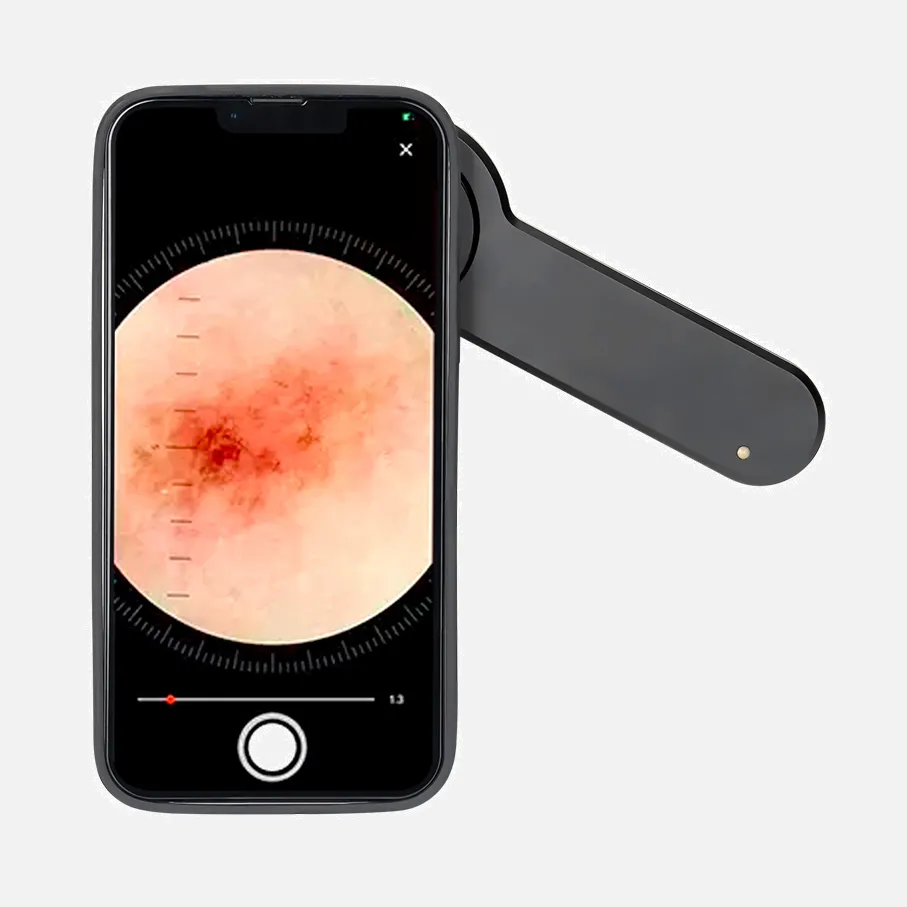
To ensure optimal lighting from the flash, it is recommended to prioritize autofocus on the lesion of concern and subsequently utilize the zoom function to enhance the view, rather than physically bringing the camera closer. If the lesion is minute, it may pose challenges for the camera to achieve a precise focus. In such cases, it is advisable to step back and reattempt the focusing process, as opposed to physically advancing the camera towards the lesion.
Why holds dermoscopy a pivotal role? It equips physicians with the capability to discern benign from malignant tumors, enabling proactive monitoring of skin lesions that may harbor cancerous potential. This ensures timely intervention, should it be deemed necessary, thereby mitigating the risk of late-stage treatment. Furthermore, dermoscopy proves instrumental in assisting clinicians in precisely defining the surgical boundaries for skin cancer excision. 3rd May, 2022
The comprehensive precision rate of dermoscopy attained a level of 73.7%. In terms of specific diagnoses, dermoscopy demonstrated a high degree of accuracy for identifying Demodex with a rate of 88.1%, scabietic conditions with 89.7%, and dermatophytic folliculitis achieving a perfect score of 100%. Additionally, it performed impressively in diagnosing pseudofolliculitis, attaining an accuracy of 92.8%.
Frequently, the development of skin cancer is observed in regions of the body that are consistently subjected to ultraviolet (UV) radiation emanating from sunlight, encompassing areas like:
The scalp.
The facial region.
The nose.
The upper parts of the ears.
The lips.
The neck.
The chest area.
The arms.
Additional body parts... •
Cancerous transformation of precancerous cells is not a certainty; it may or may not occur. Given their abnormal nature, it is crucial to keep them under surveillance or, under specific circumstances, undertake their removal to mitigate the potential risk of developing cancer in the future.
The healthcare professional applies a small amount of oil or gel onto your epidermis, facilitating the dermatoscope's operation more efficiently. Subsequently, they position the dermatoscope against your skin and examine it through the instrument. This process is entirely painless and poses no harm to your skin.
Approximately half of the consultations with dermatologists span a duration ranging from 20 to 29 minutes. Among the most frequently performed dermatological procedures lies the surgical intervention aimed at eradicating or excising premalignant growths, comprising over 14 percent of all annual dermatological procedures.
Dermatoscopic examination, also known as dermatoscopy, entails utilizing a dermatoscope for microscopic inspection of the skin's surface. This technique is predominantly employed in the assessment of pigmented skin abnormalities. Skilled practitioners find it a facilitator in diagnosing melanoma with greater ease.
Proliferation of pigmentation from the perimeter of a lesion into adjacent skin areas. Manifestation of inflammation or novel swelling extending past the mole's boundary. Variation in sensory perception, encompassing itchiness, sensitivity, or discomfort. Alterations in the mole's surface characteristics, including scaliness, exudation, hemorrhage, or the emergence of a protuberance.