Case for iPhone – IBOOLO
People May Ask
The drawbacks associated with Mohs' procedure lie in the fact that it frequently entails longer waiting periods in comparison to traditional excision methods, owing to its extended nature which often encompasses multiple stages within a single day. Furthermore, not every instance of skin cancer qualifies as a candidate for excision via Mohs' technique.
Typically, malignant cSCC tumors exhibit distinct features such as a diameter exceeding 2 centimeters, a depth greater than 5 millimeters, a propensity for high recurrence rates, perineural infiltration, as well as loco-regional metastatic spread, as documented in [22,23].
A universally accepted definition for high-risk cutaneous squamous cell carcinoma (cSCC) remains elusive. However, it is typically characterized as those instances of cSCC that pose a greater than 5% likelihood of recurrence, lymph node involvement, and/or the development of distant metastases, with the specific risk level being assessed based on the presence of certain identifying high-risk attributes.
Encountering one or several instances of sunburns, particularly severe ones that resulted in blisters during childhood or adolescence, heightens the likelihood of developing squamous cell carcinoma of the skin later in life. Furthermore, enduring sunburns even in adulthood poses an additional risk factor. Possessing a past record of precancerous skin abnormalities is also noteworthy, as certain types of skin lesions have the potential to evolve into skin cancer.
Invasive SCC lesions with a diameter measuring under 2 cm have demonstrated a metastasis rate of 9.1%, in contrast, those exceeding 2 cm in diameter exhibit a significantly higher metastatic rate, reaching up to 30.3%. April 18th, 2024.
Squamous cell carcinoma can develop in various regions of the body, yet its prevalence is notably higher in specific areas such as: the Skin, as well as the Mouth, Tongue, and Throat, collectively referred to as Oral Carcinoma.
Basaloid squamous cell carcinoma, abbreviated as BSCC, represents a formidable and infrequently encountered type of oral malignancy, standing among the scarcest and most virulent subsets of squamous cell carcinoma (SCC), the prevalent form of the disease. It often manifests as a high-grade condition, accompanied by a grim prognosis for patients.
Prompt medical attention is highly recommended for individuals diagnosed with cSCC. Given the rapid progression of Cutaneous Squamous Cell Carcinoma, a delay in treatment, even by a short span of 1–2 months, can result in an enlargement of the tumor. Fortunately, doctors are often successful in treating early-stage cSCC by eradicating or surgically removing smaller tumors.
The development of SCCs is often observed in scars, skin lesions, and various skin trauma sites. The neighboring skin typically exhibits indications of solar injury, encompassing wrinkles, alterations in pigmentation, and a reduction in elasticity. These SCCs manifest as thick, coarse, and scaly areas that may exhibit crusting or bleeding.
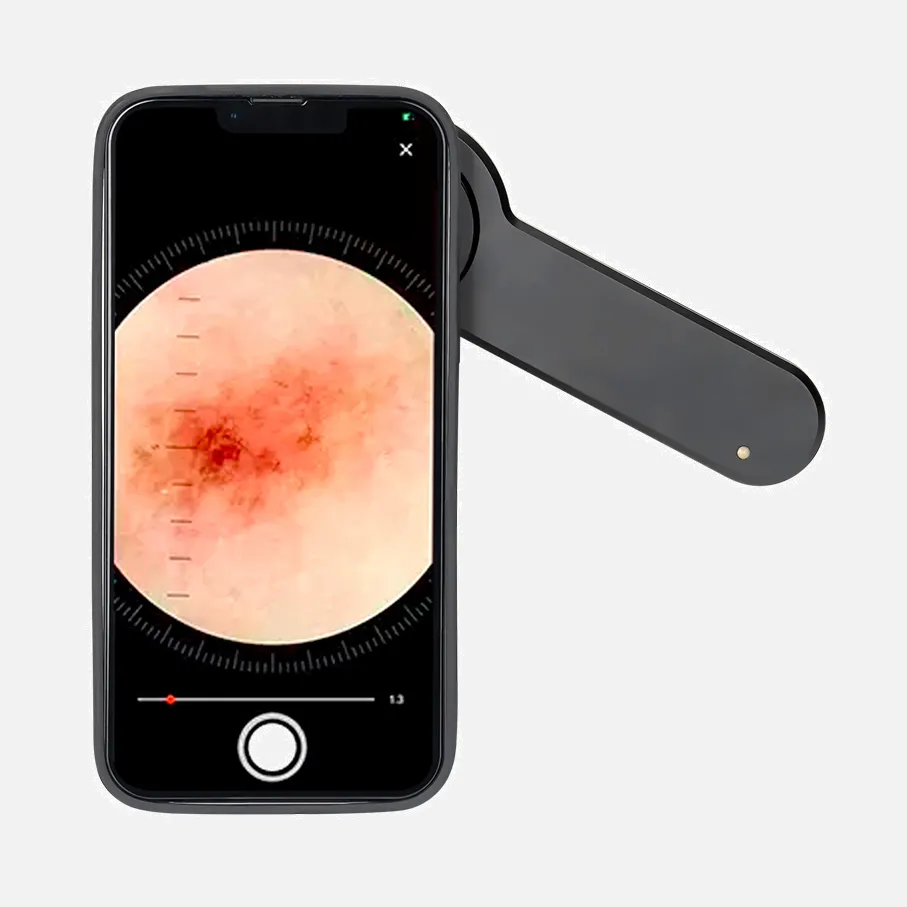
The distinctive dermoscopic characteristics of cutaneous squamous cell carcinoma encompass: Circular white patches, areas devoid of distinct structure, looped blood vessels, keratin accumulation in the center, and a pink or red underlying tissue particularly evident in tumors with poor differentiation or rapid growth.