Case for iPhone – IBOOLO
People May Ask
A patient undergoing Mohs micrographic surgery for a skin abnormality might necessitate the restoration of the affected area. The approach to reconstruction can differ significantly, contingent upon factors such as the extent of the surgical site, its anatomical position, and the individual patient's preferences. Notably, when Mohs surgery targets delicate regions like the nose, eyelids, or ears, the recommendation for reconstruction frequently arises.
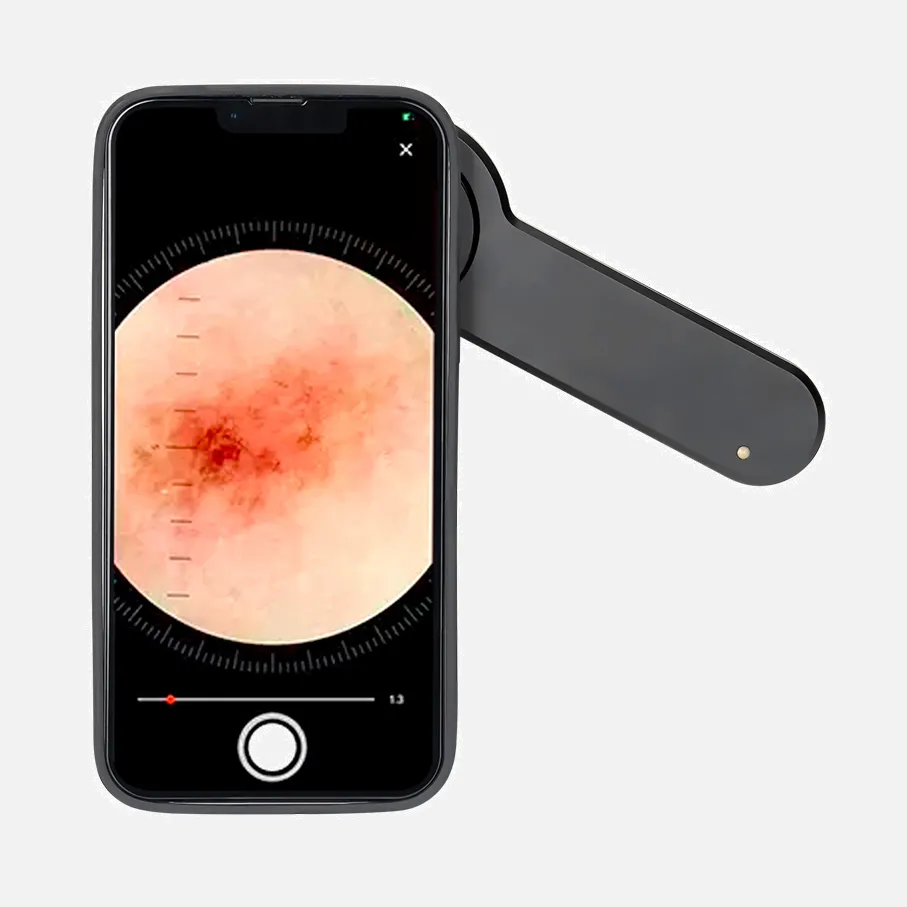
An additional crucial clue in diagnosing superficial BCC could be identified through the existence of minute ulcerations, manifesting as red to brown homogeneous areas devoid of distinct structures on dermoscopy, observed in approximately 79% of our examined lesions. Furthermore, in 15 of our 42 cases of superficial BCCs, elongated arborizing vessels were detected.
In the absence of timely treatment for basal cell carcinoma, the skin cancer is prone to a gradual expansion, infiltrating deeper layers of tissue, including muscles, bones, and cartilages. As a result, the BCC may manifest painful symptoms and ulceration, leading to bleeding and infection.
The likelihood of basal cell carcinoma disseminating via the bloodstream or lymph nodes is exceedingly uncommon, often occurring solely in cases where the cancer has been neglected for an extended period. Nevertheless, this underscores the importance of early treatment, as untreated cases can potentially infiltrate deeper, harming nerves, blood vessels, and potentially even affecting the bone.
Despite its infrequent association with mortality, basal cell carcinoma possesses the potential to inflict significant damage and distort local tissues, particularly when therapeutic intervention is inadequate or postponed. March 13th, 2024
However, if left untreated, basal cell carcinoma has the potential to progressively invade deeper layers of the skin, resulting in severe damage to adjacent tissues. In extreme cases, it can even pose a life-threatening risk. For instance, an untreated basal cell carcinoma located on the face may eventually infiltrate the bones and, with time, even reach the brain, as emphasized by Dr. [Name].
The initial indicator of basal cell carcinoma manifests as an abnormal development on the skin's surface. You might observe a nodule with a waxy texture, or a minute, smooth, glossy, or pale protrusion. Alternatively, a lump might not be present, and instead, you may discern a flat area that appears subtly dissimilar to the surrounding skin tone.
The morphological characteristics observed under dermoscopy in morphoeic basal cell carcinoma typically encompass: A dominant white, scar-resembling region devoid of distinct structures, accompanied by sparse delicate branching vessels resembling serpents, and numerous brownish speckles. On occasion, the vessels alone serve as the pivotal indicator.
What are the indicative markers of basal cell carcinoma? BCCs frequently commence as minor alterations in the skin's texture, resembling a tiny protrusion or a flattened reddish area. These changes tend to manifest on areas of the body that are regularly exposed to sunlight. Gradually, over time, they enlarge and become more conspicuous.
The utilization of liver ultrasonography (US) alongside serum alpha-fetoprotein (AFP) evaluations serves as a crucial tool for the preliminary detection of HCC, and it is advised to conduct such screenings at a frequency of no less than six-monthly intervals in high-risk demographic groups [3].