Case for iPhone – IBOOLO
People May Ask
The identification of melanoma typically commences with a straightforward visual assessment of the skin, subsequently followed by a biopsy procedure. In certain scenarios, additional imaging techniques might be deemed necessary. Initially, a dermatologist or a primary healthcare provider often conducts the skin evaluation, whereas a skilled oncologist performs the biopsy, with the subsequent analysis being undertaken by a pathologist.
It typically manifests as a flattened or marginally protruding brown lesion, exhibiting a heterogeneous pigmentation (incorporating hues such as black, blue, pink, or white discoloration) with an irregular contour, often exceeding 6mm in size.
Notably, in the context of this discussion, it is estimated that approximately 40 to 50 percent of uveal melanoma cases remain undiagnosed for more than a decade, whereas only a fraction of less than 5 percent of cutaneous melanoma exhibits such a prolonged latency.
Regrettably, a significant number of patients remain unaware of the underlying issues as melanomas progress silently, exhibiting no symptoms until the condition has escalated to a critical stage.
Melanoma, a highly concerning form of skin cancer, is characterized by the unregulated proliferation of cells responsible for the production of pigment, a compound in skin that is integral to color generation. Melanomas often arise abruptly and unexpectedly. They are predominantly observed on the face, neck, upper back, and legs, though they can manifest in any region of the body.
Melanoma does not exclusively originate as a mole, but it can also manifest in otherwise unblemished skin. Symptoms of melanoma can arise anywhere on the body, most frequently in regions that have undergone sun exposure.
Although melanoma is relatively infrequent compared to other skin cancer varieties, it poses a significant threat due to its high propensity to disseminate to other bodily regions if undetected and untreated in its early stages. October 27th, 2023
Despite advancing to stage 4, melanoma remains responsive to surgical intervention, chemotherapy, radiation therapy, immunotherapy, and/or precision-targeted therapy. Nevertheless, once the malignancy disseminates, the identification and management of all cancerous cells may become a challenging task. 10th July 2019
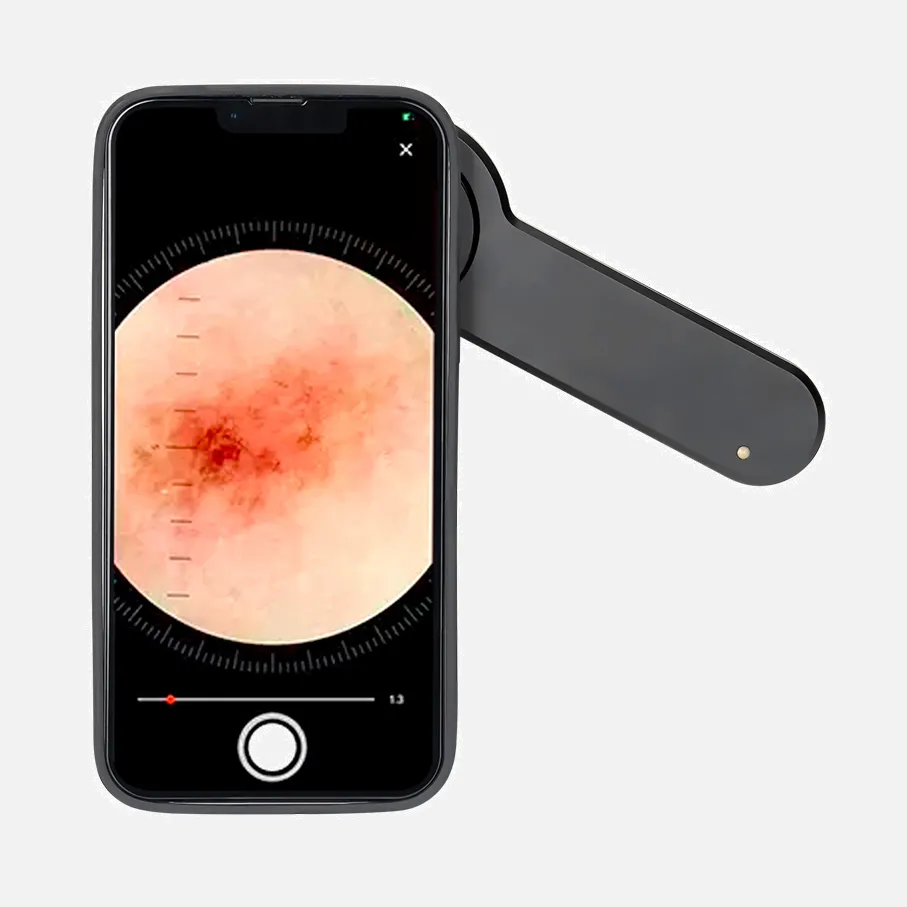
When selecting a dermatoscope, several crucial factors deserve consideration: Compatibility: Compatibility with smartphones and cameras is essential. Polarization Options: One must decide between polarized, linear-polarized, unpolarized, or variable polarization. Viewing Modes: Determining whether contact or non-contact viewing, or perhaps a combination of both, is suitable for one's needs. Magnification Capabilities: Consider the range of magnifications available, such as 10x, 16x, or 40x. Additional Considerations: There are numerous other factors to take into account as well.
While seborrheic keratosis does not progress into melanoma, the two skin conditions can be confounded due to their similar visual characteristics. Both exhibit brown or black hues and can manifest anywhere on the body. However, there are crucial distinctions to be noted: Seborrheic keratoses tend to occur in clusters, whereas melanoma typically presents as a solitary lesion.