Case for iPhone – IBOOLO
People May Ask
The medical terminology for a mole is designated as nevus. These nevi are benign in nature and can either be present from birth, referred to as congenital, or they can develop postnatally, categorized as acquired. Some nevi manifest in a raised form, while others remain flat. The color spectrum of these moles is diverse, encompassing hues ranging from the natural skin color to pink, tan, brown, black, and occasionally even blue.
The manifestation in clinical settings is uncommon, adhering frequently to the ABCDE criteria established for melanoma, which encompass asymmetry, borders displaying irregularity, diverse coloration, a significant diameter (exceeding 6 millimeters), and the presence of a lesion that progresses over time. As these nevi exhibit atypical characteristics, they are frequently subjected to biopsy due to the heightened concern they evoke regarding the possibility of atypical moles or melanoma.
Should there be any alterations observed in their appearance, be it in terms of color, form, dimensions, or border, or if you encounter a lesion that refuses to heal, it is imperative to consult a dermatologist promptly. Additionally, any newly emerged moles that arouse your suspicion should be subjected to a thorough examination by your dermatologist.
Benign nevi are typically monochromatic, varying in hue from skin tone to a deep brown. Their shape tends to be circular or elliptical. Furthermore, these benign moles exhibit symmetry, meaning that when bisected, both halves exhibit a similar appearance. Most melanocytic nevi measure approximately the size of a pencil eraser or smaller.
The integration of shearing procedures alongside electrocautery and curettage has emerged as a reliable and efficient approach for managing intradermal nevi. Additionally, this technique stands out as a more straightforward, cost-effective, and rapidly acquirable option in comparison to traditional methods of nevus eradication.
The two most prevalent eyelid tumors, distinguished by their nature, are intradermal nevus (IDN) and basal cell carcinoma (BCC), where the former is benign and the latter is malignant. IDN, a harmless condition, arises from the typical multiplication of nevomelanocytes, often necessitating no therapeutic intervention. Conversely, BCC, a cancer known for its gradual progression, poses a risk of localized damage if left untreated.
A dermal nevus represents a benign skin lesion that is distinctly visible, elevated, and pigmented, presenting itself as a papule on the epidermal layer. These nevi can exhibit a diverse array of colors, including but not limited to brown, tanned, black, reddish-brown, purple hues, or even mimicking the natural skin tone. Typically, they take on a round or ovoid shape, and may either be flat-based or elevated, with the possibility of hair follicles sprouting from their surface.
A nevus, which is a common skin lesion, manifests as a minute protrusion on the skin, typically displaying hues of pink, tan, or brown and possessing a well-defined boundary. Conversely, a dysplastic nevus tends to be larger in size and lacks a circular or oval contour, as well as a clear-cut perimeter. It may exhibit a blend of pink, tan, or brown tints. Posted on 13 October 2011.
Minor nevi can effectively be eliminated through straightforward surgical procedures. The nevus tissue is excised, and the neighboring skin is sutured together, resulting in a minimal scar. However, in the case of a large congenital nevus, the affected skin area necessitates substitution.
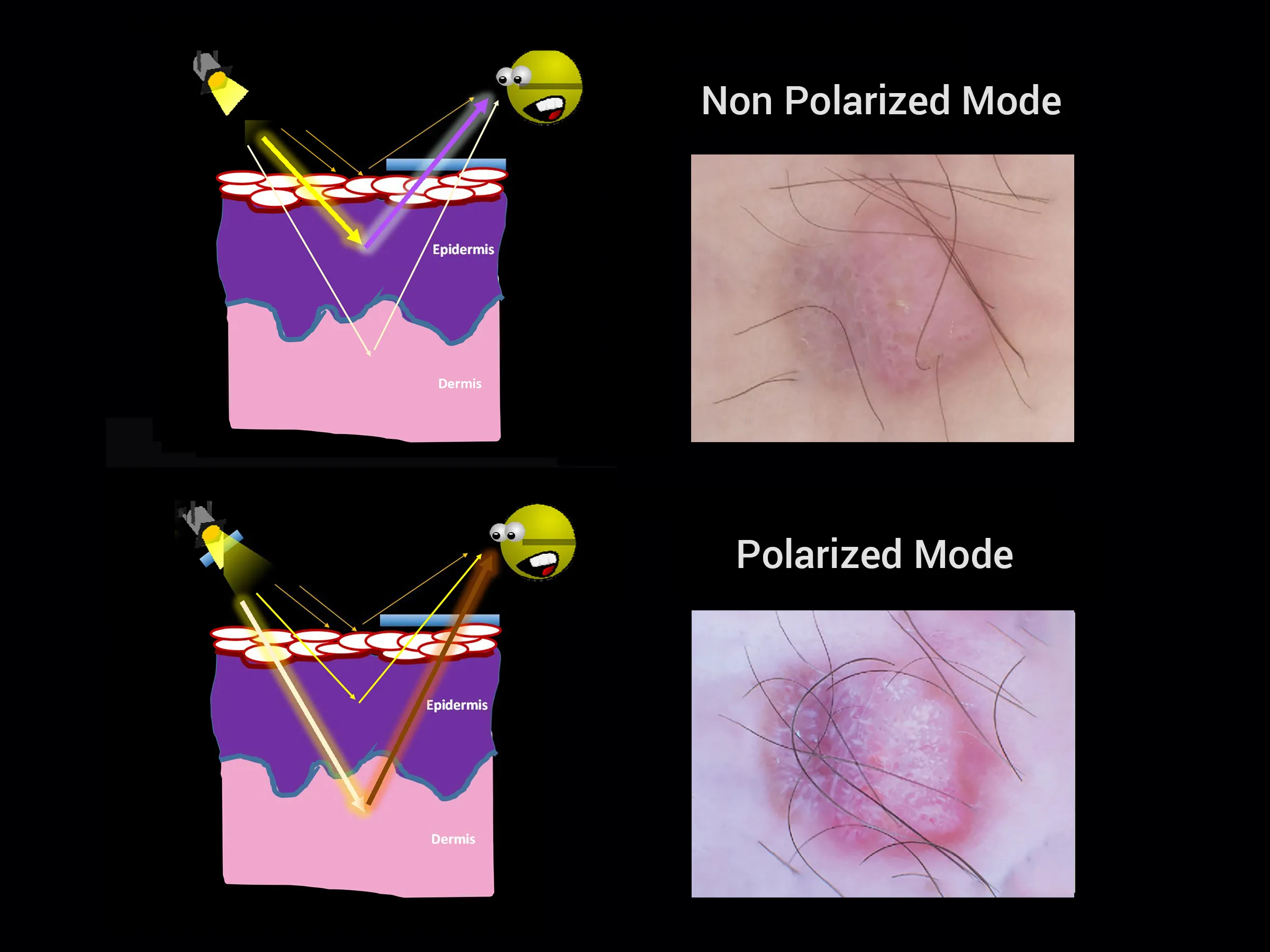
A dermal or intradermal nevus exhibits clusters of nevus cells embedded within the dermis. These manifestations can present as papules, plaques, or nodules, with varying surface features such as pedunculated protrusions, papillomatous structures reminiscent of Unna nevus, or a smooth texture akin to Miescher nevus. Furthermore, a compound nevus is characterized by the presence of nevus cell clusters not only at the epidermal-dermal interface but also distributed throughout the dermis.