Dermatology UV 365nm & 405nm DE-315 Woods Lamp
Dermatology UV 365nm & 405nm DE-315 Woods Lamp
- 4.5 x Magnification
- 60mm Lens Diameter
- 20 LEDs (10 UV 365nm, 10 Uv 405nm)
- 2 Types Colour Lighting
- Automatic shutdown
- Ultra long life battery
|
Lens Diameter |
50mm |
|
Magnification |
4.5X |
|
Ultraviolet Wavelength |
365nm&405nm |
|
Radiation Intensity |
3.5 mW/cm2 |
|
Battery Capacity |
2000mAh |
|
Charging |
USB Type-C |
|
Working Time |
2-6 hours |
|
Dimensions |
240mm*100mm*34mm(L*W*H) |
What It Has
- 365nm UV Light:A Wood's lamp has broadband light
sources that emit light at wavelengths between 320nm
and 400nm, with a peak at 365nm. - 405nm UV Light:Fluorescence Excitation
- 4.5X Magnification:Low distortion magnify
- 2000mAh Battery: Offering up to 6 hours long time and stable diagnosis.
In The Box
- DE-315 Woods Lamp
- USB Type-C Charging Cable
- Microfiber Cloth
- User Manual
Specs
- Lens Diameter:50mm
- Magnification:4.5X
- Ultraviolet Wavelength: 365nm & 405nm
- Radiation Intensity: 3.5 mW/cm2
- Battery Capacity:2000mAh
- Charging:USBType-C
- Working Time:2-6 hours
- Dimension:240mm*100mm*34mm(L*W*H)
Premier 365nm UV Lamp & Woods Lamp Suppliers - IBOOLO
IBOOLO suppliers offer professional 365nm UV Lamps and Woods Lamps for advanced dermatological diagnosis. Features dual 365nm & 405nm UV wavelengths, 4.5X magnification, and 6-hour battery life.
Woods Lamp & 365nm UV Lamp: A Comprehensive Guide for Dermatology Professionals and Suppliers
In the ever-evolving field of dermatology, both Woods Lamps and 365nm UV Lamps stand out as crucial diagnostic tools. This comprehensive guide explores these essential devices, and their applications in dermatology, and provides valuable information for practitioners and suppliers.
What is a Woods Lamp and 365nm UV Lamp?
A wood lamp, also known as a Wood Lamp or blacklight, along with specialized 365nm UV Lamps, are diagnostic tools used in dermatology. They emit long-wavelength ultraviolet light (UV-A) specifically in the 365 nanometer range, which can reveal features and conditions of the skin not visible under normal light.
Key Features:
- UV-A light emission (precise 365nm wavelength)
- Portable design
- Long bulb life
- Minimal heat production
- Various sizes and models available
History and Development
The Woods Lamp was invented by physicist Robert Williams Wood in 1903. Initially used in physics experiments, its application in dermatology was discovered in the 1920s. Since then, it has become an indispensable tool in dermatological practices worldwide, with modern 365nm UV Lamps representing the latest evolution in this technology.
Applications in Dermatology
Woods Lamps and 365nm UV Lamps have a wide range of applications:
1. Pigmentation Disorders: Identifying conditions like vitiligo and melasma
2. Bacterial Infections: Detecting certain bacterial infections like erythrasma
3. Fungal Infections: Diagnosing fungal infections such as tinea capitis
4. Porphyria: Assessing porphyrin production in various types of porphyria
5. Sun Damage: Evaluating the extent of sun damage and pigmentation changes
6. Hair Disorders: Examining hair shafts for certain conditions
7. Professional Skin Analysis: 365nm UV Lamps provide precise wavelength examination
8. Clinical Documentation: Specialized 365nm UV photography for treatment tracking
How They Work
These devices function by emitting UV-A light, with 365nm UV Lamps providing particularly precise wavelength control. Different conditions produce different colours of fluorescence: Bacterial infections: Coral red, Fungal infections: Pale blue-green, Porphyrins: Pink to orange-red, Normal skin: Dull blue.
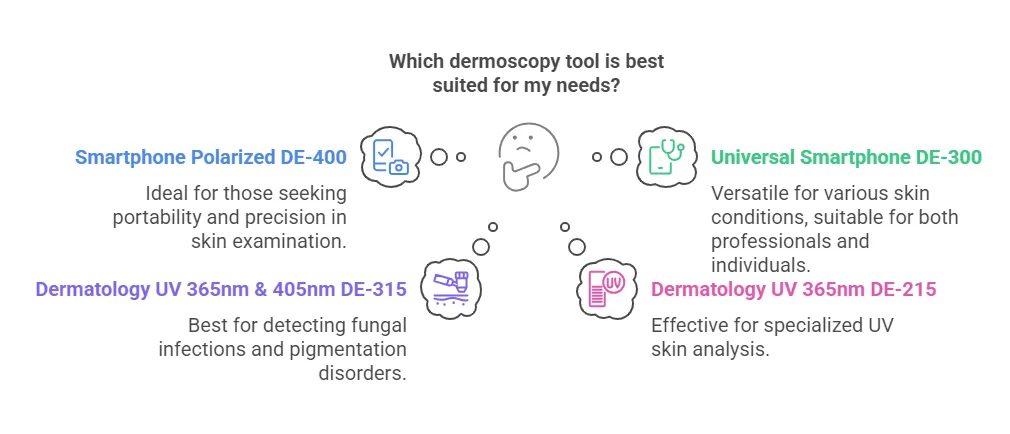
Comparing Diagnostic Tools
While both Woods Lamps and 365nm UV Lamps are valuable, they're often used alongside other tools:
1. Traditional Woods Lamps: Broader spectrum examination
2. Precision 365nm UV Lamps: Targeted wavelength analysis
3. Handheld Dermatoscopes: Higher magnification
4. Digital Imaging Systems: Documentation
Choosing the Right Equipment
When selecting equipment, consider: Light intensity and wavelength accuracy, Portability and size, Durability and build quality, Additional features (e.g., magnification lenses), Price and warranty, Wavelength precision (especially for 365nm UV Lamps), Clinical application requirements, Integration capabilities.
Finding the Right Supplier
Consider these factors when choosing a supplier:
1. Product Range: Various models including both Woods Lamps and 365nm UV Lamps
2. Quality Assurance: Certified products meeting medical standards
3. Customer Support: Excellent service and technical support
4. Pricing: Competitive rates with quality assurance
5. Warranty and Maintenance: Comprehensive coverage
6. Reputation: Strong standing in the medical community
Maintenance and Care
Proper maintenance ensures longevity and effectiveness: Regular cleaning with appropriate disinfectants, Timely bulb replacement, Proper storage in cool, dry conditions, Careful handling to prevent damage.
The Future of Dermatological UV Diagnosis
As technology advances, we can expect: Enhanced wavelength precision, Digital integration capabilities, Combined diagnostic platforms, Improved spectral analysis, Integration with other diagnostic tools.
Whether you're a dermatologist, medical facility manager, or supplier, understanding both Woods Lamps and 365nm UV Lamps is crucial in modern healthcare. These tools continue to evolve while remaining fundamental to dermatological diagnosis and treatment planning.
Recommended reading
Account – IBOOLO
Shenzhen Iboolo Optics Co.Ltd founded in 2012,is located in the beautiful city of Shenzhen, Guangdong. Our main products including Microscope, Woods Lamp, Macro lens and Dermatoscope, etc.
amelanotic melanoma dermoscopy – IBOOLO
IBOOLO is a camera lens manufacturer based in China with more than 11+ years of experience in manufacturing, catering to a variety of requirements. We have become experts in the design and manufacture of a wide variety of Dermatoscope, Microscope, Macro lens and Woods Lamp.
Cart – IBOOLO
Shenzhen Iboolo Optics Co.Ltd has been specialized in researching and manufacturing industrial Woods Lamp, Dermatoscope, Macro lens and Microscope, since 2012. As a professional smartphone lens supplier, we have excellent teams who focus on products development & design, quality control & inspection and company running.
Clinical Applications
The Wood's lamp is used to identify the extent of pigmented or depigmented patches and to detect fluorescence. Normal healthy skin is slightly blue but shows white spots where there is thickened skin, yellow where it is oily, and purple spots where it is dehydrated. Clothing lint often shines bright white.
What Makes it Unique
Woods lamps use ultraviolet light to reveal skin abnormalities that can’t be seen with human eyes. Build with 60mm field view and no cross-infection design, this Woods lamp can be held about 10-30 cm away from the skin for detection. The examination is painless and safe.
You might also like
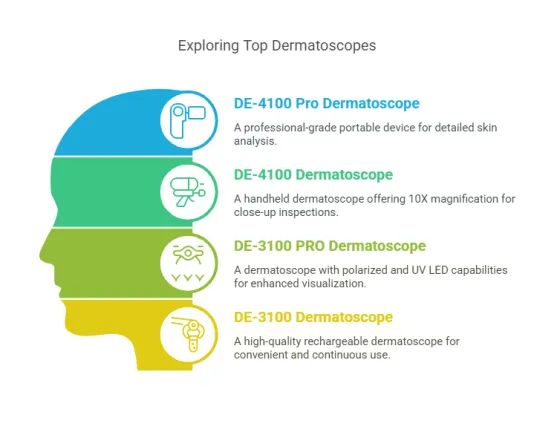
DE-4100 Dermatoscope
$699.00
DE-3100 Dermatoscope
$499.00
DE-400 Dermatoscope
$179.00
DE-300 Dermatoscope
$99.00
Reviews
1 review for DE-315 Woods Lamp
Only logged in customers who have purchased this product may leave a review.
Learn More
IBOOLO Dermatoscope Accessories
What Are the Available Accessories for IBOOLO Dermatoscopes? When it comes to enhancing the functionality of your IBOOLO dermatoscope, there are several accessories available to suit different needs. These include…
The Best Dermoscopy Tools: A Comprehensive Guide to Top Devices for Skin Examination
Dermoscopy is an essential technique for examining skin lesions, enabling early detection of conditions such as melanoma, fungal infections, and pigmentation disorders. With the evolution of dermoscopy tools, both professionals…
The Best Dermatoscopes: A Comprehensive Guide to Top Models
Dermatoscopes are essential for dermatologists, medical professionals, and even individuals interested in skin health monitoring. With advanced technology, these devices allow for detailed examination of skin lesions, aiding in the…









































Damian Nowak Poland
–
Poland
–
High-quality product, very bright light, totally recommend