Article
Melanoma under Dermoscopy
Under dermoscopy, malignant melanoma can often be characterized by atypical pigment networks, irregular dot-ball shapes, and a bluish-white veil. For a clear view, the physician needs to clean the patient’s skin area under observation in advance and adjust the dermoscopic focus until the lesion is magnified to the appropriate size. Through dermoscopy, doctors can detect…
Clinical Guide: Identifying Melanoma and Melanoma In Situ Under Dermoscopy
In the field of cutaneous oncology, the accuracy of dermoscopy melanoma screening is the cornerstone of reducing mortality. As a non-invasive diagnostic technique, dermoscopy provides a window into the microscopic morphological structures of the skin, bridging the gap between clinical examination and histopathology. For clinicians, the ability to identify the subtle dermoscopic features of melanoma at its earliest stage—particularly melanoma in situ dermoscopy—is a life-saving skill.
At IBOOLO, we understand that professional diagnostics require superior optical resolution. This guide explores the complex patterns of melanoma under dermoscopy and provides clinical insights to enhance diagnostic confidence.
Mastering Melanoma In Situ Dermoscopy: The Earliest Clues
Diagnosing melanoma in situ dermoscopy remains one of the greatest challenges in dermatology. Because the tumor cells are confined to the epidermis, the features are often discrete and can easily be mistaken for atypical nevi.
Key markers to observe in situ cases include:
- Atypical Pigment Network: Look for irregular meshes and lines that vary in thickness, often with abrupt peripheral termination.
- Regression Structures: Fine blue-gray granules (peppering) that indicate the body's immune response to early malignant cells.
- Asymmetric Follicular Openings: Especially in lentigo maligna (facial in situ), where pigment accumulates asymmetrically around the hair follicles.
Essential Dermoscopic Features of Invasive Melanoma
As melanoma evolves and invades the dermis, the dermoscopic features of melanoma become more chaotic and disorganized. Analyzing dermoscopy images of melanoma requires a focus on structural chaos:
- Blue-White Veil: A hazy, grayish-blue area representing deep dermal pigment or focal orthokeratosis. This is a high-specificity marker for invasive melanoma.
- Irregular Streaks and Pseudopods: Finger-like projections at the lesion's edge, indicating active radial growth.
- Atypical Vascular Patterns: The emergence of "corkscrew," "dotted," or "linear-irregular" vessels, reflecting neoangiogenesis required for tumor progression.
- Polychromasia: The presence of 5-6 different colors (black, brown, gray, blue, red, white) distributed haphazardly within a single lesion.
Comparison: Benign Nevus vs. Melanoma Under Dermoscopy
Differentiating malignant lesions from benign moles is the primary clinical application of the dermatoscope. The table below summarizes the key threshold differences.
| Diagnostic Feature | Benign Nevus | Malignant Melanoma |
|---|---|---|
| Structural Symmetry | High (Symmetrical) | Low (Chaotic/Asymmetric) |
| Pigment Network | Uniform and Fading | Atypical and Broadened |
| Vascular Pattern | Typically Absent | Polymorphous / Irregular |
| Specific Structures | Regular Globules | Blue-White Veil / Pseudopods |
Optimizing Clinical Observation with High-Resolution Imaging
The reliability of identifying melanoma under dermoscopy is fundamentally tied to the quality of the optical system. High-resolution imaging provided by IBOOLO professional dermatoscopes allows clinicians to resolve the "fine peppering" and "atypical vessels" that might be missed by lower-grade equipment.
By utilizing cross-polarization and digital smartphone integration, clinicians can capture and store dermoscopy images of melanoma for longitudinal monitoring. This "Sequential Digital Dermoscopy Imaging" (SDDI) is particularly vital for identifying the "E" (Evolving) criteria in early-stage lesions, ensuring timely intervention while reducing unnecessary biopsies of benign lesions.
Mastery of dermoscopy melanoma protocols is an essential clinical competency. By integrating high-performance optical tools with a systematic pattern-recognition approach, clinicians can achieve diagnostic accuracy exceeding 90%.
Recommended reading
Custom Download DE-4100 User Manual suppliers & factories – IBOOLO
IBOOLO is a Custom Download DE-4100 User Manual suppliers & factories. Information for Download DE-4100 User Manual: DE-4100 user manualDownload...
dermoscopy of actinic keratosis – IBOOLO
Shenzhen Iboolo Optics Co.Ltd was established in 2012, It has been engaged in the field of Dermatoscope, Microscope, Macro lens and Woods Lamp etc. IBOOLO is a professional camera lens manufacturer with more than 11+ years experiences, which is located in Shenzhen, Guangdong.
Cart – IBOOLO
Shenzhen Iboolo Optics Co.Ltd has been specialized in researching and manufacturing industrial Woods Lamp, Dermatoscope, Macro lens and Microscope, since 2012. As a professional smartphone lens supplier, we have excellent teams who focus on products development & design, quality control & inspection and company running.
Under dermoscopy, malignant melanoma can often be characterized by atypical pigment networks, irregular dot-ball shapes, and a bluish-white veil. For a clear view, the physician needs to clean the patient’s skin area under observation in advance and adjust the dermoscopic focus until the lesion is magnified to the appropriate size. Through dermoscopy, doctors can detect abnormalities in the early stages of melanoma, which can lead to timely intervention and treatment and reduce unnecessary harm.
Melanoma Basics
Melanoma is a type of skin cancer that develops in the skin cells called melanocytes. It can be found in the head and neck, trunk and extremities. Based on its histologic type, it is classified into the following main types: superficial diffuse melanoma, nodular melanoma, malignant freckle melanoma, and limb freckle melanoma.
Melanoma accounts for about 6.8% to 20% of cutaneous malignancies and is one of the more common tumors of the skin. It develops in adults, especially in middle-aged and elderly people. Fair-skinned Caucasians have a relatively high incidence, while dark-skinned Asians and Africans have a lower incidence. Exposure to ultraviolet light is an important predisposing factor for melanoma. Prolonged or intense UV exposure may damage melanocytes in the skin, thereby increasing the risk of melanoma.
Introduction to Dermoscopy
Dermoscopy is an instrument based on optical principles to observe the morphology and texture of the skin surface. Firstly, the skin of the area to be examined needs to be cleaned, and appropriate observation modes, such as amber light mode, polarized light mode, etc. Finally, the dermatoscope is placed on the skin of the area to be examined for observation.
Dermoscopy can clearly observe the morphology, color, boundary and other characteristics of the skin lesion, which helps doctors more accurately determine the nature and type of the lesion, thus improving the diagnostic accuracy of melanoma.

Preparation for Dermoscopy
Prior to dermoscopy, the patient should clean and dry the skin at the examination site, and the physician should choose between different types of dermoscopies (hand-held or digital) depending on the site and purpose of examination. Light in the test process should be uniform and moderate, not dazzling and shadows. They need to be aware of the principle of aseptic work and should be provided with sterile equipment and sterilized dermatoscope cleaned carefully before each patient in order to decrease the risk of infection.
How to Recognize Melanoma under Dermoscopy?
Melanomas demonstrate atypical pigment networks, irregular streaks, blue–white structures and irregular blood vessels in situ dermoscopy. The ABCDE rule is a guide to help you recognize melanoma.
A (Asymmetry) asymmetry: melanoma is usually asymmetric with irregular borders to the surrounding normal skin.
B (Border) Border: The border of a melanoma is usually unclear, showing jagged, irregular or fuzzy edges.
C (Color): Melanomas may be unevenly colored and present in a variety of colors.
D (Diameter): Melanomas are usually larger than 6 millimeters in diameter.
E (Evolution) Evolution: Melanomas can change over time, such as increasing in size, changing in color, developing itching, breaking down, etc.
Can dermatoscopy examine melanoma on all parts of the body?
Dermoscopy allows doctors to observe small changes in the surface of the skin and examine various parts of the body for skin pigmented diseases, such as malignant freckle-like nevus on the head and neck, superficial diffuse melanoma on the trunk area, nail melanoma and mucosal melanoma on the extremities. However, for deeper or complex melanomas, further skin biopsy may be required to identify them due to their complex structure.
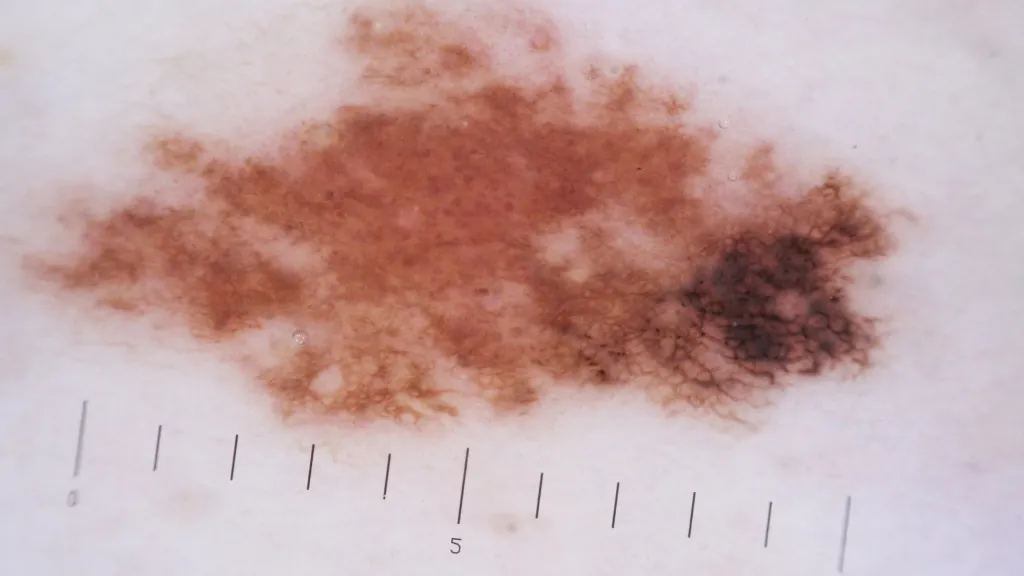
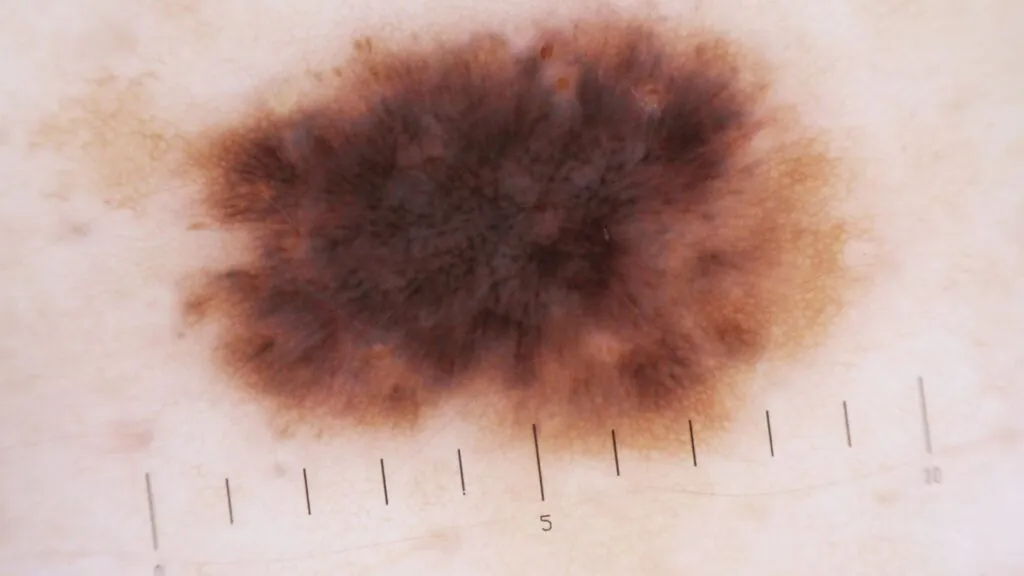
Dermoscopy Images of Melanoma
Melanoma has a variety of specific patterns dermoscopically, including: atypical pigment networks, irregular streaks, irregular dots and balls, irregular stains, and blue-white curtains.
A patient, female, 59 years old, had a family history of malignant melanoma. An asymmetric, irregular brown patch, approximately 7 x 6 mm, was found on the right leg. dermoscopic images showed typical melanoma features-irregular streaks, irregular dots and balls, irregular stains, and blue-white curtains, among others. The final diagnosis was malignant melanoma
Challenges and limitations of Dermoscopy
Melanoma in its early stages may manifest only as very small changes in skin color, and these changes may be difficult to accurately capture in situ dermoscopy. Some specific types of melanoma, such as limbal freckle-like melanoma or malignant freckle-like nevus-type melanoma may resemble benign lesions, leading to misdiagnosis. Moreover, the diagnostic accuracy of dermoscopy is highly dependent on the experience and skill level of the examiner, and inexperienced physicians may have difficulty accurately recognizing the dermoscopic features of melanoma.
Integration of Dermoscopy with Other Diagnostic Methods
Dermoscopy can be used as a complementary tool to clinical assessment, helping doctors to more accurately observe features such as the shape, color, luster and distribution of skin lesions. When dermoscopy reveals suspected malignant lesions or when the nature of the lesion cannot be determined, it can be combined with skin biopsy for further diagnosis.
Situ dermoscopy can be combined with clinical assessment, skin biopsy and other methods to form a multidisciplinary collaborative diagnostic model. This helps to provide a comprehensive understanding of the condition from multiple perspectives, improving diagnostic accuracy and therapeutic efficacy.
The Role of Dermoscopy in the Early Detection of Melanoma
Dermoscopy is an advanced diagnostic tool for skin imaging, which utilizes optical principles to magnify the microscopic structure of the skin surface, enabling physicians to observe the features of melanoma more clearly. Moreover, it is non-invasive, convenient and intuitive without causing any damage to the patient’s wound.
In addition to relying on specialized medical equipment and doctors for diagnosis, raising public awareness of skin health and self-examination is also an important means of preventing skin diseases such as melanoma. Hospitals or related professionals popularize skin health knowledge to the public, including the prevention of skin diseases such as melanoma, through various channels such as the media, the Internet, and community lectures.
Clinical Case Study of Dermoscopy
Patient Situation: The patient was a middle-aged male who presented to the clinic with the finding of a progressively larger black plaque on his back.
Initial Examination: The doctor first performed a visual observation and found that the black plaque on the patient’s back was irregular in shape, with different shades of color and blurred edges, initially suspecting that it might be a melanoma.
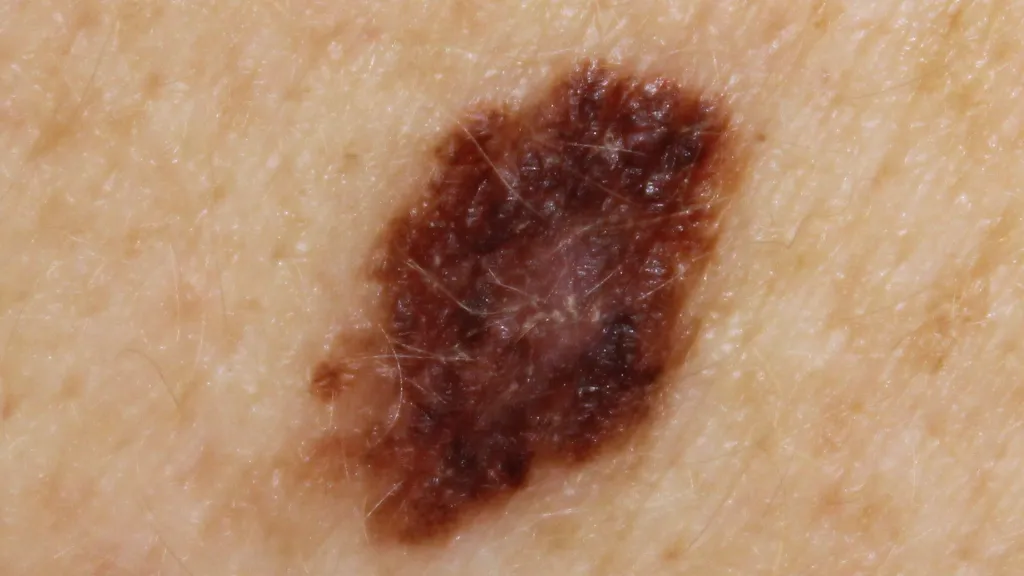
Dermoscopy: Under dermoscopy, the doctor observed a complex network of pigmentation within the plaque, as well as multiple blue-white structures and irregularly distributed spheres and dots.
Diagnostic Findings: To confirm the diagnosis, the doctor recommended a skin biopsy. The biopsy resulted in melanoma.






















