Article
Medical Dermatoscopes
As a dermatologic diagnostic tool, dermoscopy is mainly used in dermatology to examine skin diseases, and can observe minute skin changes that are not detectable by the naked eye, helping doctors to diagnose various skin problems more accurately. Conventional dermoscopy techniques use a non-polarized light source and often require the application of a medium (e.g.,…
Medical Dermatoscopes: Essential Dermatoscope Uses | IBOOLO
IBOOLO professional medical dermatoscopes for accurate skin diagnosis. Explore dermatoscope uses in clinical examination and early detection of skin conditions.
Medical Dermatoscopes uses: Advanced Tools for Precise Skin Examination
In modern dermatology practice, medical dermatoscopes uses have become indispensable tools for accurate skin examination and diagnosis. These sophisticated devices enable dermatologists to observe minute skin details that are invisible to the naked eye, revolutionizing how we detect and diagnose various skin conditions.
Understanding Medical Dermatoscopes and Their Evolution
Medical dermatoscopes have transformed significantly from their early iterations. Today's advanced devices feature polarized light technology, eliminating the need for contact fluids while providing crystal-clear visualization of subsurface skin structures. These modern medical dermatoscopes typically offer 10x to 20x magnification, enabling practitioners to examine skin lesions with unprecedented detail.
Essential Dermatoscope Uses in Clinical Practice
Healthcare providers employ dermatoscope uses across various clinical scenarios:
1. Skin Cancer Screening: Early melanoma detection, Non-melanoma skin cancer assessment, Monitoring of suspicious lesions.
2. General Dermatological Assessment: Inflammatory skin conditions, Hair and scalp disorders, Vascular lesions.
3. Documentation and Monitoring: Progress tracking, Treatment response evaluation, Patient education.
Advanced Features of Modern Medical Dermatoscopes
Current-generation medical dermatoscopes incorporate several key technological advances: Cross-polarized lighting systems, High-resolution digital imaging capabilities, Wireless connectivity for image sharing, Integrated measurement tools, Mobile device compatibility.
Clinical Applications and Patient Benefits
The versatility of dermatoscope uses extends across multiple clinical applications: Non-invasive examination methodology, Real-time analysis capabilities, Enhanced diagnostic accuracy, Improved patient communication, Treatment planning optimization.
Technology Integration and Future Developments
The future of medical dermatoscopes lies in their integration with emerging technologies: Artificial intelligence assistance, Cloud-based image storage, Telemedicine compatibility, 3D mapping capabilities, Advanced image analysis tools.
Best Practices for Dermatoscope Implementation
To maximize the effectiveness of medical dermatoscopes in clinical practice:
1. Regular staff training
2. Standardized examination protocols
3. Proper device maintenance
4. Systematic documentation
5. Quality control measures
Medical dermatoscopes continue to evolve as essential tools in dermatological practice. Understanding various dermatoscope uses and implementing them effectively can significantly enhance diagnostic accuracy and patient care quality. As technology advances, these devices will become even more integral to dermatological practice, particularly in early detection and monitoring of skin conditions.
Recommended reading
Blog – IBOOLO
Shenzhen Iboolo Optics Co.Ltd is an experienced manufacturer& exporter in the field of camera lens. Our main products include Dermatoscope, Macro lens, Microscope and Woods Lamp. We keep developing varieties of our products and upgrading our quality control systems to enhance our markets competitiveness.
China Manufacturer & Factory Specializing in Professional Dermoscopy Models - IBOOLO
Through engineering mastery nurtured over a decade, our China manufacturer & factory produces Professional dermoscopy devices combining sturdy builds and unmatched optics for flexible precision skin analysis.
amelanotic melanoma – IBOOLO
Founded in 2012, Shenzhen Iboolo Optics Co.Ltd focuses on the camera lens, we are providing Dermatoscope, Microscope, Macro lens and Woods Lamp with very competitive price and service.
As a dermatologic diagnostic tool, dermoscopy is mainly used in dermatology to examine skin diseases, and can observe minute skin changes that are not detectable by the naked eye, helping doctors to diagnose various skin problems more accurately. Conventional dermoscopy techniques use a non-polarized light source and often require the application of a medium (e.g., gel) to the skin to prevent the effects of reflections on the skin surface during observation. This is relatively cumbersome and susceptible to ambient light. On the other hand, modern medical dermatoscopes have a polarized light pattern that prevents gross reflections on the skin surface allowing to observe tiny skin details without medium imposition. Medical dermatoscopes also typically have higher magnification, allowing for a clearer view of skin structures.
Definition and Importance of Medical Dermoscopy
Medical dermoscopy has a wide range of applications in the field of dermatologic medicine. Dermoscopy can assist in the diagnosis of a variety of skin tumors. Many pigmented diseases also require the use of dermoscopy, including vitiligo, apatite, anemia, and so on. Doctors can also use dermoscopic images of androgenetic alopecia to determine the type of alopecia and to assess follicular atrophy.
Dermoscopy is able to put in-depth observation of the structure under the stratum corneum and even the superficial dermis, observing details that cannot be observed by the human eye and improving the accuracy of diagnosis of skin lesions.
Technical Characteristics of Medical Dermoscopy
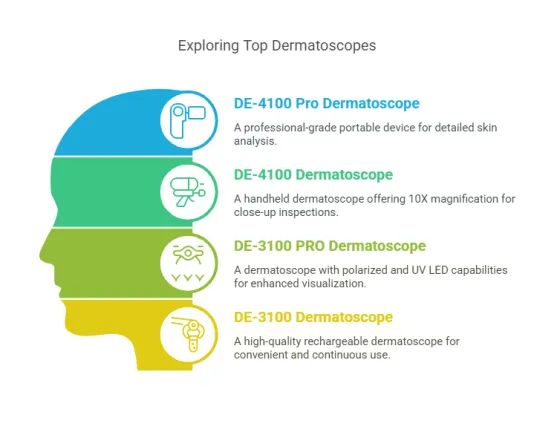
The IBOOLO Medical Dermatoscope DE-4100 has a magnification of 10X and is available in white, polarized, amber and white-mixed amber to provide a very clear field of view with the naked eye.The DE-4100 can also be easily attached to a cell phone and camera using the IBOOLO magnetic phone case or magnetic threaded ring to save images while observing.

Dermoscopy Uses
Dermoscopy uses are extensive in dermatological examinations. By magnifying skin tissues, dermoscopy reveals changes in skin blood vessels and pigmentation, assisting doctors in making more precise diagnoses of skin conditions. Dermoscopy has a wide range of applications, primarily used for examining various skin lesions on the body, such as seborrheic dermatitis, pityriasis rosea, and molluscum contagiosum. Additionally, during clinic visits, doctors can observe the fine structures on the skin’s surface and even detect potential skin cancer lesions. For instance, melanoma often appears under dermoscopy with jagged, irregular, or blurred borders, often accompanied by blue-white globules.
The Role of Medical Dermoscopy in Skin Cancer Screening
Early-stage skin cancer is usually confined to the surface of the skin or superficial tissues. Through timely treatment, such as surgical excision and photodynamic therapy, the condition can be effectively controlled and prevented from further deterioration. The treatment of early skin cancer is relatively simple and the treatment cost is relatively low. Therefore, early detection and treatment are of great importance in reducing the psychological and economic burden of patients.
And dermoscopy has an irreplaceable role in early screening of skin cancer. Dermoscopy is easy to operate, takes less time for examination and has high magnification. This makes dermoscopy ideal for large-scale skin screening programs.

Impact of Medical Dermoscopy on Patient Care
As a non-invasive examination tool, medical dermoscopy does not cause any discomfort to the client during the examination. Especially for patients with ulcerated skin lesions, dermoscopy can provide clear dermatoscopic images without ensuring any contact with the patient’s skin. This greatly reduces patient pain and helps increase patient satisfaction and trust. Moreover, patients can gradually learn to use dermoscopy for self-examination by themselves under the educational guidance of their doctors and observe their recovery in real time.
Guidelines for the Operation of Medical Dermoscopy
Before using a dermatoscope, it is necessary to disinfect and sterilize the patient’s skin area to be observed and ensure that the skin is dry. Then, place the dermatoscope above the skin to be observed and adjust the focus until the field of view is clear. After each use, disinfect the contact surface of the dermatoscope’s probe to prevent cross-infection. Additionally, during storage, a lens cap should be worn to avoid scratching or damaging the lens.
Training and Education in Medical Dermoscopy
Medical dermoscopy is only a testing tool, the diagnosis still needs the judgment of the doctor, experienced doctors can often give accurate judgment results based on dermoscopic images. Doctors who have just started to enter the clinic naturally need to receive continuous training from the hospital, grow their experience in practice, and grow into a doctor who can make reasonable judgments. Only in this way can a virtuous circle be formed to promote the sustainable development of dermatology.

The Use of Dermoscopy in the Diagnosis of Specific Skin Lesions
Dermoscopy allows visualization of pigmentary changes in the epidermis, reticular layer of the dermis, and changes in the vasculature of the superficial mesodermis. This technique has been widely used for the early diagnosis of malignant melanoma and differential diagnosis with other cancers. Dermoscopy can also assist in the diagnosis of a variety of inflammatory diseases such as lichen planus, psoriasis, follicular keratosis, and urticarial vasculitis. Dermoscopy is able to differentiate scarring alopecia from non-scarring alopecia, and the common forms of pemphigus vulgaris and alopecia areata can also be visualized in dermoscopic images.
Innovations and Future Trends in Medical Dermoscopy
With the application of AI in various fields, future electronic dermatoscopes will be integrated with big data models. Through continuous learning by artificial intelligence, future dermatoscopes will possess skin analysis capabilities. By utilizing image matching and data analysis, dermatoscopes can predict the type and nature of skin lesions, aiding doctors in making more accurate diagnoses. Additionally, they can dynamically collect patient information and transmit it to remote experts for diagnosis, enabling patients in medically underserved areas to access high-quality dermatological services. As technology continues to advance, portable dermatoscope devices will become more widespread, serving as important tools for home self-monitoring and health management.
Key Uses and Benefits of Dermoscopy
Medical dermoscopy is an important tool in modern dermatologic diagnosis and is widely used in clinical diagnosis. Dermoscopy is easy to operate, has a short detection time and relatively low cost, making it suitable for widespread use in dermatology outpatient clinics. It is also non-invasive and does not cause damage to the skin, which makes it highly acceptable to patients. With the development of technology, dermoscopy will have a wider and wider range of applications and higher accuracy.