Article
Dermoscopy Seborrheic Keratosis
Seborrheic keratosis, also known as senile warts, age spots or basal cell papillomas, is a benign skin tumor that is prevalent in middle-aged and older adults. Seborrheic keratoses are typically benign, never becoming malignant. They don’t become cancerous in most cases. They are painless, although they may itch or become inflamed from friction and other…
Seborrheic keratosis, also known as senile warts, age spots or basal cell papillomas, is a benign skin tumor that is prevalent in middle-aged and older adults. Seborrheic keratoses are typically benign, never becoming malignant. They don’t become cancerous in most cases. They are painless, although they may itch or become inflamed from friction and other soreness. Although seborrheic keratoses are harmless in and of themselves, their appearance may sometimes resemble malignant melanoma. Then we can rule out the risk of skin cancer by taking a closer look at the comparison using the ultra-clear magnification of a dermatoscope.
What Is Seborrheic Keratosis?
These are Seborrheic keratosis, also know as senile warts or seb ksage spotsker. The appearance of seborrheic keratosis is linked to the functioning process and a range of circumstances which counts on skin aging, hereditary history, as well mutations in gene increasing sensitivity its genes light exposure. Seborrheic keratosis is prevalent in middle-aged and older adults, especially those over 50 years of age. The incidence of the disease increases with age. Epidemiologic surveys show that 80-100% of people over 50 years of age in Asia suffer from seborrheic keratosis.
Initially, seborrheic keratosis is characterized by light brown patches that are well demarcated. As the disease progresses, the patches may gradually increase in size and become flat papules or plaques, with a rough surface and deepening color to dark brown or even black.
Subtypes of seborrheic keratoses can be broadly categorized into classic acanthosis nigricans, reticular seborrheic keratoses, agitated seborrheic keratoses, hyperkeratotic seborrheic keratoses, verrucous seborrheic keratoses, pigmented seborrheic keratoses, and acanthoma nigricans pigmented seborrheic keratoses.

Principles and Development of Dermoscopy
Dermoscopy, based primarily on the principle of optical magnification, which magnifies the image of the skin surface 20-200 times by means of a set of magnifying lenses, or lenses. With the development of technology, portable handheld dermatoscopes are becoming popular, and the built-in cross-polarized light system makes the examination more convenient.
Dermoscopy is able to visualize subtle structural and pigmentary changes that cannot be detected by the naked eye, thus significantly improving the diagnostic accuracy of skin diseases. Especially for the early diagnosis of malignant melanoma and other serious skin diseases is of great significance.
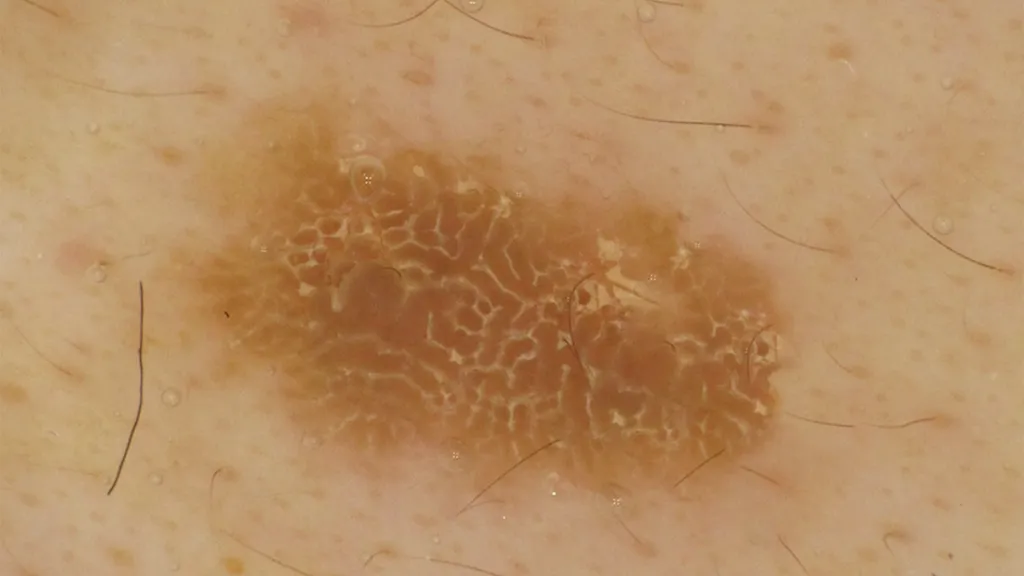
Dermoscopic Features of Seborrheic Keratoses
Milia-like cysts: white, creamy white or yellow round structures that are keratin-filled cysts within the epidermis.
Comed-like openings: round to ovoid keratin-filled fissures that may appear brown, orange, yellow, or black.
Brain-like or cerebriform pattern: a curved thick line of keratin-filled furrows and gyrus, also known as furrow ridge structures.
Hairpin blood vessels: a semi-annular or hairpin-like structure formed by two parallel linear vessels, often surrounded by a white halo, as a result of proliferation of keratin-forming cells.
Blue-gray globules: similar structures may be observed in clonal seborrheic keratosis CSK or in mixed manifestations with other skin lesions.
Punctate vessels: Punctate vasculature appears as dermoscopic punctate red or purple dots that may reflect changes in the superficial skin vasculature.
Seborrheic Keratoses and Other Skin Lesions
Seborrheic keratoses: tend to be flat, plaque-like lesions with well-defined borders and being generally smooth in consistency. It has even pigment spread and very few large pigmented alterations.
Melanoma: irregular margins, variegation of color, often poorly circumscribed and may have areas that ulcerate or bleed. There is often a mixture of black, brown, red and other colors.
Basal cell carcinoma: lesions commonly have pearly raised edges, the center is at times to be ulcerated and very often pigmentation will not equal throughout.
Dermoscopy is a non-invasive skin imaging technique which allows detailed microstructural information of the skin lesions and thus helps in increasing diagnostic specificity. Under dermoscopy, therefore it is highly sensitive in diagnosing as well. It can help in identifying and indicating areas of suspicious lesions earlier by examining the pigmentation pattern, vascular structure, keratinization degree etc., which may contribute to cure or early treatment.
How to Recognize Seborrheic Keratosis Pilaris?
The use of dermoscopy allows for clearer visualization of the microstructure of the lesions, thus differentiating between the two. Melanoma shows irregular vascular patterns, uneven pigment distribution, and other features on dermoscopy, whereas seborrheic keratoses show typical gyrus-like or papilloma-like structures.
Seborrheic keratoses are most common in middle-aged and elderly people, especially in sun-exposed areas such as the face, back of the hands, and forearms. The characteristic manifestations of seborrheic keratosis can be further confirmed by dermoscopy.
How to Use Dermoscopy Results for Clinical Decision Making?
Skin cancer should be highly suspected when dermoscopic findings show lesions with features of malignant lesions, at which point biopsy should be recommended for definitive diagnosis. Based on the biopsy results, the nature of the lesions should be clarified and the corresponding treatment plan should be formulated. For benign lesions, such as seborrheic keratosis, laser, freezing, surgical excision and other methods can be used for treatment; for malignant lesions, such as melanoma, individualized and comprehensive treatment plans should be formulated according to the staging and grading of the tumor.

Diagnosis of Seborrheic Keratosis
Background: A 55-year-old man presented with an irregular dark brown plaque on his right calf that had lasted for more than 4 years.
Dermoscopic examination: light to dark brown spherules were scattered around the periphery of the lesion, the spherules were irregularly shaped, and a cobblestone-like structure was seen at the edge of the lesion, with an eccentric hypopigmented area and a well-defined lesion border.
Interpretation: Light to dark brown spherules are one of the common dermoscopic manifestations of seborrheic keratoses. The lesions are well demarcated, and the cobblestone-like structures at the margins may reflect hyperkeratosis and irregularity of the lesion surface.
Treatment and Management of Seborrheic Keratoses
For the clinical seborrheic keratosis treatment, cryotherapy is one of the most common methods. The method is to freeze the skin lesion tissue using liquid nitrogen and other low-temperature refrigerants, causing local tissue necrosis that ultimately leads it off in sections.
Which laser to utilize for treatment depends on thickness and type of the lesions as well. There is typically no scarring or minimal risk of post-inflammatory pigmentary changes following treatment.
Cryo or laser treatment, it needs to be taken care of correctly afterwards. Patients should avoid water to keep the wound dry and clean to prevent infection. Patients need to perform regular follow-up in accordance with the doctor’s instructions so that doctors can observe treatment results and adjust future treatments. Feel uncomfortable —— consult your doctor.

Prevention and Health Education
Strategies for preventing seborrheic keratosis mainly include sun protection and regular skin examinations, while educating patients on skin self-examination is also crucial.
Ultraviolet light is one of the main factors that induce and aggravate seborrheic keratosis, so reducing UV damage to the skin is the key to preventing the disease. And regular skin checkups can help detect seborrheic keratosis or other underlying skin problems at an early stage so that timely treatment measures can be taken. In a well-lit area, use a tool such as a dermatoscope to look carefully at the skin all over the body. If you notice any changes in spots or moles on the skin, record them and seek medical advice.






















