Article
Dermoscopy of Superficial Basal Cell Carcinoma
Basal cell carcinoma is the most common skin cancer. Basal cell carcinoma rates have jumped sharply in the last years, particularly North America, Europe and selected parts of Asia. As BCC is slow-growing, then the majority are curable and cause little harm if diagnosed early and treated. Accompanied by the advances in medical technology, dermoscopy…
Superficial Basal Cell Carcinoma Dermoscopy: Key to Diagnosis - IBOOLO
Dermoscopy identifies Superficial Basal Cell Carcinoma features like arborizing vessels, aiding accurate diagnosis and early treatment. A vital tool for skin cancer management.
Dermoscopy for Superficial Basal Cell Carcinoma: A Key Tool for Precise Diagnosis and Treatment
Superficial basal cell carcinoma (SCBC) is a common skin tumour that often presents diagnostic challenges due to its similarity to benign conditions like eczema or psoriasis. Dermoscopy, a non-invasive imaging technique, has emerged as a critical tool in the management of superficial basal cell carcinoma dermoscopy by magnifying skin lesions and revealing characteristic features such as arborizing vessels and leaf-like areas. This article explores the role of superficial basal cell carcinoma dermoscopy in-depth, covering its working principles, diagnostic advantages, clinical applications, limitations, and the latest research advancements. By providing a comprehensive overview, we aim to highlight the significance of this technology in improving the diagnosis and treatment of SBCC.
What is Dermoscopy for Superficial Basal Cell Carcinoma and Why Does It Matter?
Superficial basal cell carcinoma (SBCC), a subtype of basal cell carcinoma, typically appears as red patches or scaly lesions, often on the trunk or limbs. Its clinical presentation can mimic benign conditions such as eczema or psoriasis, making accurate diagnosis essential. Superficial basal cell carcinoma dermoscopy offers a non-invasive solution by magnifying the lesion and allowing clinicians to observe distinctive features like arborizing vessels, leaf-like areas, and superficial erosions. This enables earlier and more precise identification of SBCC, reducing the risk of misdiagnosis and ensuring timely treatment.
The clinical significance of superficial basal cell carcinoma dermoscopy lies in its ability to enhance diagnostic accuracy. Providing high-resolution visualization of skin structures, it empowers dermatologists to differentiate SBCC from other conditions, paving the way for effective management strategies.
How Does Dermoscopy Work in Superficial Basal Cell Carcinoma Diagnosis?
Superficial basal cell carcinoma dermoscopy operates by amplifying the skin’s surface and subsurface structures, typically between 10x and 100x magnification. It employs polarized light or a liquid interface (like alcohol or gel) to minimize surface reflections, revealing details of the epidermis and upper dermis. For SBCC, the technique highlights key features such as:
1. Magnification of Details: It exposes subtle patterns like branching vessels and surface irregularities.
2. Contrast Enhancement: Polarized light reduces glare, making vascular and structural features stand out.
3. Image Documentation: Captured images allow for analysis, comparison, and follow-up.
This technical foundation makes superficial basal cell carcinoma dermoscopy an indispensable tool for identifying and managing sBCC effectively.
Why is Dermoscopy Crucial for Superficial Basal Cell Carcinoma?
The importance of superficial basal cell carcinoma dermoscopy stems from its ability to address the diagnostic challenges posed by sBCC’s variable presentation. Unlike traditional visual inspection, dermoscopy reveals specific markers that set sBCC apart from other skin conditions. Common dermoscopic features of sBCC include:
- Arborizing Vessels: Elongated, branching blood vessels, a hallmark of SBCC.
- Leaf-like Areas: Well-defined, brown or grey structures resembling leaves.
- Superficial Ulcers: Small erosions or crusting on the lesion’s surface.
By identifying these patterns, superficial basal cell carcinoma dermoscopy reduces unnecessary biopsies and misdiagnoses, ensuring patients receive appropriate care.
How to Perform Superficial Basal Cell Carcinoma Dermoscopy
Conducting superficial basal cell carcinoma dermoscopy requires a systematic approach:
1. Prepare the Lesion: Clean the area with a mild cleanser to remove oil and debris.
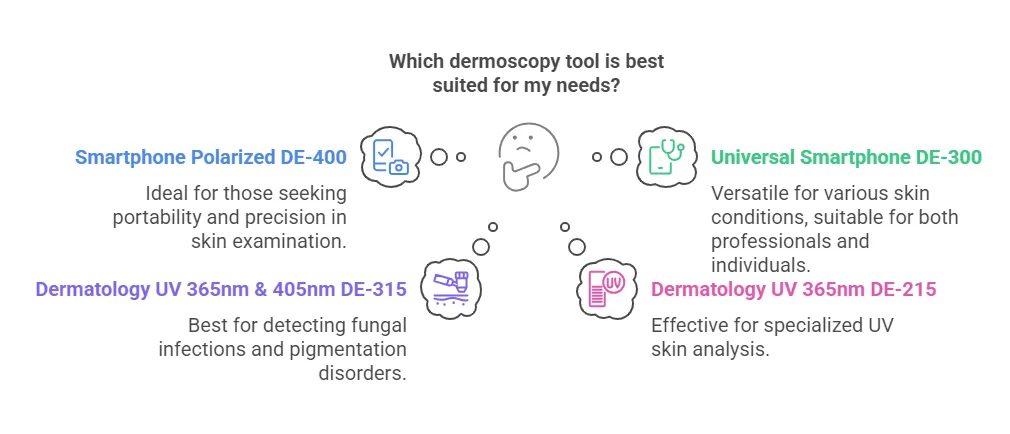
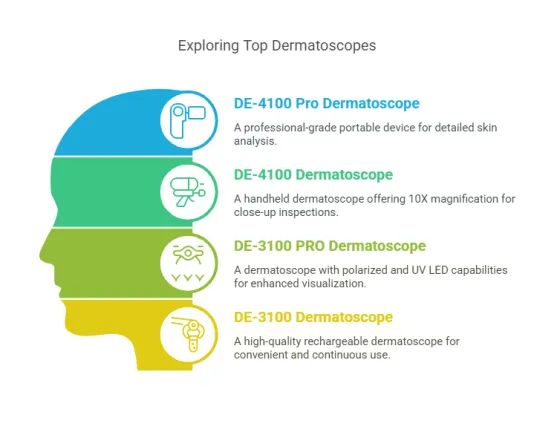
2. Select Equipment: Choose a handheld or desktop dermoscope based on the lesion’s size and location.
3. Apply a Coupling Agent: Use alcohol or gel to reduce surface reflection.
4. Examine Features: Observe vascular patterns, surface structures, and borders under magnification.
5. Document Findings: Capture images and note key characteristics for analysis and records.
This structured process ensures that superficial basal cell carcinoma dermoscopy yields reliable results, supporting accurate diagnosis and treatment planning.
Can Dermoscopy Enhance the Diagnosis of Superficial Basal Cell Carcinoma?
Superficial basal cell carcinoma dermoscopy significantly improves diagnostic precision by offering detailed insights into lesion characteristics. For instance:
- Eczema Differentiation: Eczema shows dotted vessels and scaling, while sBCC features arborizing vessels and leaf-like areas.
- Psoriasis Differentiation: Psoriasis displays uniform dotted vessels and white scales, contrasting with sBCC’s irregular vascular patterns.
By highlighting these distinctions, superficial basal cell carcinoma dermoscopy minimizes diagnostic errors, enabling clinicians to confidently identify sBCC and avoid unnecessary interventions.
What Are the Clinical Benefits of Dermoscopy for Superficial Basal Cell Carcinoma?
Superficial basal cell carcinoma dermoscopy offers several advantages in clinical practice:
- Non-Invasive: It eliminates the need for immediate biopsies, reducing patient discomfort.
- High Accuracy: Specific features enhance diagnostic reliability.
- Early Detection: It identifies sBCC at an early stage, preventing progression.
- Treatment Monitoring: Post-treatment dermoscopy assesses lesion response, guiding further management.
These benefits position superficial basal cell carcinoma dermoscopy as a cornerstone of sBCC care.
Does Dermoscopy Have Limitations in Superficial Basal Cell Carcinoma Diagnosis?
While highly effective, superficial basal cell carcinoma dermoscopy has limitations: Atypical Lesions, Some sBCC cases lack classic features, complicating identification. Operator Dependence, Accuracy relies on the clinician’s expertise. Equipment Quality, Low-resolution devices may compromise image clarity. In ambiguous cases, histopathological confirmation remains necessary, complementing superficial basal cell carcinoma dermoscopy findings.
Key Dermoscopic Features of Superficial Basal Cell Carcinoma
Superficial basal cell carcinoma dermoscopy reveals distinct characteristics that aid diagnosis:
- Leaf-like Areas: Sharp-edged, pigmented structures.
- Superficial Ulcers: Minor erosions or crusts.
- Lack of Pigmentation: Unlike melanoma, sBCC typically shows minimal melanin.
Arborizing Vessels: Long, branching vessels.
These hallmarks make superficial basal cell carcinoma dermoscopy a powerful diagnostic ally.
How to Differentiate Superficial Basal Cell Carcinoma from Other Lesions with Dermoscopy
Superficial basal cell carcinoma dermoscopy facilitates differentiation from similar conditions: Eczema, Dotted vessels and scales vs. sBCC’s arborizing vessels. Psoriasis, Uniform dotted vessels and white scales vs. sBCC’s irregular patterns. Melanoma, Irregular pigmentation and varied vessels vs. sBCC’s consistent lack of pigment. This clarity reduces misdiagnosis risks, enhancing patient outcomes.
Maintenance and Care of Dermoscopy Equipment for Superficial Basal Cell Carcinoma
Proper upkeep of dermoscopy tools ensures consistent performance in superficial basal cell carcinoma dermoscopy:
1. Clean the Lens: Use a specialized cloth and solution to remove debris.
2. Check Lighting: Replace bulbs or batteries as needed.
3. Avoid Damage: Handle with care to prevent drops or impacts.
4. Store Properly: Keep in a dry, clean environment.
5. Calibrate Regularly: Seek professional calibration for precision.
These steps preserve the reliability of superficial basal cell carcinoma dermoscopy.
Latest Advances in Dermoscopy for Superficial Basal Cell Carcinoma
Recent research has elevated superficial basal cell carcinoma dermoscopy: AI Integration and machine learning algorithms now assist in feature recognition, reducing errors. High-resolution imaging and advanced dermoscopes enhance the visualization of subtle details. Combined Technologies, Pairing dermoscopy with optical coherence tomography (OCT) offers deeper insights. These innovations promise even greater precision in sBCC management.
Superficial basal cell carcinoma dermoscopy is a transformative tool in dermatology, offering a non-invasive, accurate means of diagnosing and managing sBCC. By revealing features like arborizing vessels and leaf-like areas, it distinguishes sBCC from benign conditions, supports early detection, and aids treatment evaluation. Despite limitations such as operator dependence, ongoing advancements—like AI and high-resolution imaging—continue to enhance its utility. For clinicians, mastering superficial basal cell carcinoma dermoscopy through training and quality equipment is key to optimizing patient care. This comprehensive guide underscores its vital role in improving sBCC outcomes.
Recommended reading
High Quality Dermoscopy Meaning Created in Our Products Supply Based in China - IBOOLO
Our China products supply hub couples world-class portability with elite precision, using seasoned expertise to develop high quality dermoscopy meaning for flawless skin visualization anywhere through compact size.
China 365nm UV Lamp Manufacturer & Factory Provides Affordable Products for Clients - IBOOLO
As a leading 365nm UV Lamp manufacturer & factory in China, we specialize in affordable products to meet our clients' unique needs. Our skilled engineers can modify designs or create new UV lamps from scratch.
China Manufacturer & Factory Specializing in Professional Dermoscopy Models - IBOOLO
Through engineering mastery nurtured over a decade, our China manufacturer & factory produces Professional dermoscopy devices combining sturdy builds and unmatched optics for flexible precision skin analysis.
Basal cell carcinoma is the most common skin cancer. Basal cell carcinoma rates have jumped sharply in the last years, particularly North America, Europe and selected parts of Asia. As BCC is slow-growing, then the majority are curable and cause little harm if diagnosed early and treated. Accompanied by the advances in medical technology, dermoscopy as a non-invasive optical diagnostic tool is playing an ever-growing role for detecting superficial basal cell carcinoma at early stage.
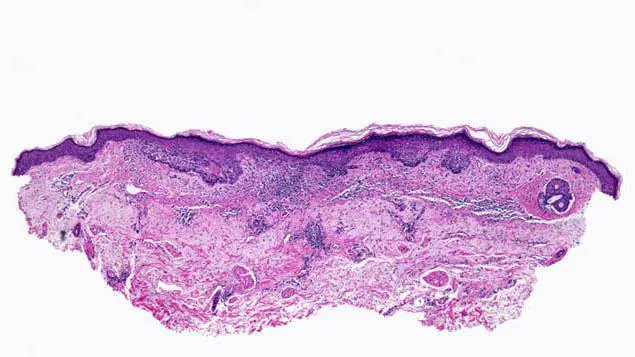
What is superficial basal cell carcinoma?
Basal cell carcinoma often referred to as basaloid is the most common type of skin cancer. It starts as a basaloid low-grade malignancy of the basal layer of epidermis or outer root sheath of hair follicles. Morphologically from clinical standpoint basal cell carcinoma can be mostly classified as: nodular-ulcerative type, superficial type, pigmented like. Basal cell carcinoma has multifactorial causes, but many cases have demonstrated a clear association with chronic sun exposure and ionizing radiation. Superficial basal cell carcinoma, a subtype of BCC that presents as red, scaly plaques on the skin, often resembling eczema or psoriasis.
Basal cell carcinoma can present in diverse clinical manifestations. The texture of these lesions tends to be firm, the surface is smooth or slightly elevated as well with a noticeable pigmentation. Basal cell carcinomas are most common on the head and neck, where they almost always affect sun-exposed areas; such as around your nose, eyelids or cheeks.

Dermoscopic features of basal cell carcinoma
Dermoscopy is useful in detecting the specific features of BCC. Some common dermoscopic characteristics are as follows:
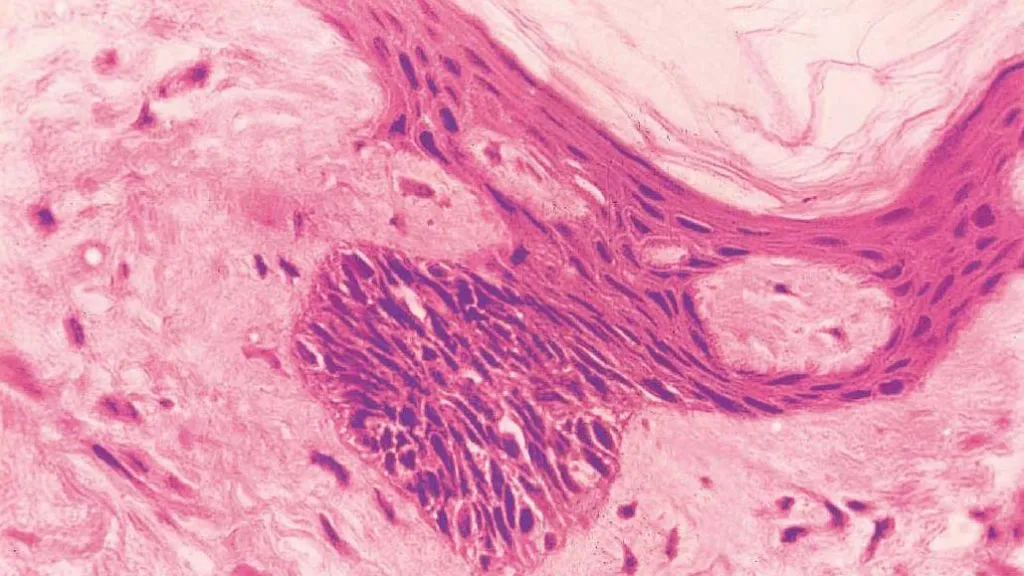
Dendritic blood vessels: Most classic dermoscopic presentations of BCC include dendritic blood vessels, which are often found in the superficial and nodular types on this lesion.
Blue-gray globules: These blobs are round or oval structures, varying in size but relatively homogeneous, and blue-gray in color on dermoscopic examination. They indicate the presence of melanin within the tumor and are commonly seen in hyperpigmented basal cell carcinoma.
Ulcers: Ulcers represent breaks or flat depres- sions in the skin, and they are observed on dermoscopy as areas of structurelessness that can appear red to orange.
Crusting: A crust is a hard cover that forms on the surface of ulcers. A crust, a yellowish or brown spot at the center of the lesion.
Superficial basal cell carcinoma features
Clinicopathological study to differentiate if a basal cell carcinoma is superficial, the morphology and growth pattern of each lesion should be evaluated. Superficial basal cell carcinomas often present as a single or multiple mildly infiltrating, erythematous scaly plaque that grows slowly and largely limits itself to the epidermis.
The often seen superficial basal cell carcinoma on the trunk, especially the back. The superficial form appears as a flat, thin red or pink patch while the sclerosing shape is characterized by thick patches that are flesh-colored or light rose and resemble scars to some extent.

Differential diagnosis of basal cell carcinoma
By dermoscopy basal cell carcinoma commonly demonstrates a pink-to-red structureless area with or without central ulceration/armor. They are more common in older individuals and usually appear on parts of the body that get lots of sun. Clinically, basal cell carcinoma is a multifaceted and multiform disease that can make subtyping challenging.
Dermoscopically melanomas have an irregular structure and shape in a multitude of colors particularly reds, blues and blacks. Although most melanomas are larger than 6 mm in diameter, early lesions can mimic benign pigmented nevi but not be noticed by the naked eye.
Dermoscopically squamous cell carcinoma has a squamous surface with visible keratin. Squamous cell infiltrative growth can be misleading to benign skin lesions such as keratosis pilaris.
Dermoscopic features and diagnostic difficulties in atypical basal cell carcinoma
Sclerosing basal cell carcinoma:
Features: white, without structure, with small twining serpentine blood vessels and many brown spots.
Challenge: Scar-like frequently and hard to differentiate from a benign scar or other sclerotic disorders.
Superficial basal cell carcinoma:
Features: fine translucent rolled margin, scattering of microerosions and mild scaling.
Challenge: Similar to inflammatory skin conditions such as eczema or psoriasis.
Cystic Basal Cell Carcinoma:
Features: soft jelly-like contents with a translucent appearance.
Challenge: confused with benign cystic lesions.
Clinical applications of dermoscopic images
Dermatoscopic images can aid in accurate sampling of biopsies when they need to be done and also decrease the unnecessary number. Characteristics of skin lesions in dermoscopy images enable experienced doctors to provide diagnoses of the type of skin cancer, and plan appropriate treatments for patients with a high speed. Furthermore, dermoscopy as a hand-held and non-invasive instrument can be easily used by the doctors to exam patients during their subsequent visits without serious of invasions that offers no discomforts for the patient; thus it may help improving compliance from patients.
The important role of dermoscopy in the treatment of basal cell carcinoma
Treatment options depend on the site and stage of the cancer, and surgery with or without adjuvant radiotherapy plays a major role in resectable basal cell carcinoma. The mainstay of treatment for limited basal cell carcinoma is surgery, and radiotherapy may be used in adjacent and complex areas, but metastatic patients will not have any hope other than benefit from systemic drug therapy.
The significance of dermoscopy in the early detection of superficial basal cell carcinoma
Many moles are invisible and some changes can only be visualized by dermoscopy, so patients should undergo routine comprehensive skin evaluation, especially of sun-exposed skin surfaces. Dermoscopy has new implications in the prevention and early diagnosis of superficial basal cell carcinoma. Dermoscopy allows visualization of the surface of skin lesions and subepidermal structures that are not visible to the naked eye through optical magnification, immersion or polarized lenses. Skin lesions revealed by dermoscopy results can be detected and managed as potentially cancerous skin lesions prior to higher cancer risk or under/over-treatment.
Patient education and self-examination
If you have a wound on your skin that has not healed after a few weeks, or if you experience redness, swelling, please seek medical attention promptly. This can be an early sign of skin cancer. In your daily life, pay attention to whether there are any new moles growing on your skin. You can use a dermatoscope to observe any changes in their size, shape, color, or texture, and promptly visit a hospital for examination if there are any abnormalities.