Article
Dermoscopy of Squamous Cell Carcinoma
Squamous cell carcinoma is not a life-threatening skin cancer to most patients. Because it usually grows and spreads slowly. But if left untreated or found late, squamous cell carcinoma can grow deep and larger, even spread to other parts of the body, like nerves, blood vessels, tissues, bones and so on. It will bring challenges…
Squamous cell carcinoma is not a life-threatening skin cancer to most patients. Because it usually grows and spreads slowly. But if left untreated or found late, squamous cell carcinoma can grow deep and larger, even spread to other parts of the body, like nerves, blood vessels, tissues, bones and so on. It will bring challenges and difficulties to cure squamous cell carcinoma,and bring serious and deadly result. Sometimes, it will cause dangerous complications. There is a high cured rate of squamous cell carcinoma if detected and treated early and timely. So, it is really important to use dermoscopy to identify and diagnose squamous cell carcinoma in early.
What is squamous cell carcinoma?
As reported, squamous cell carcinoma takes up 20 percent of skin cancer all over the world. Squamous cell carcinoma is a very common type of skin cancer that associated with overexposure of UV rays. Overexposure of UV rays usually may bring uncontrollable growth of squamous cells in the epidermis of the skin, the top layer of the skin. When the squamous cell starts to grow uncontrollably and wildly, a squamous cell carcinoma can develop. The presentation of squamous cell carcinoma is usually a firm mass with a scaly top, but ulceration may also occur. Squamous cell carcinoma can occur both on the skin and in the organs, like head, arms, legs, mouth, lungs, anus and so on, and it can happen in anywhere of the body.
What does squamous cell carcinoma look?
Depending on which places squamous cell carcinoma is located in, the symptoms can be completely different. The common manifestations of these disorders are:
A hard bump on the skin, which may be brown, pink, red or black.
Rough or scaly red (or darker) patches that may crust, ache, or bleed.
A raised growth or mass, sometimes having a lower central area called a central depression.
Open sores (areas that may ooze or scab) do not heal, or come back after healing, bleeding or itching.
Thickened wart-like skin, squamous hyperplasia skin.
What are types of squamous cell carcinoma?
According to the amount and places where squamous cell carcinoma located, here several squamous cell carcinomas are classified as below:
Cutaneous squamous cell carcinoma: Cutaneous squamous cell carcinoma is a kind of squamous cell carcinoma happens on the skin. It is also called as squamous cell skin cancer and squamous cell carcinoma of the skin. This tumor usually occurs in the epidermis (out) layer of the skin. And it also will be invasive to the out layer of the skin.
Metastatic squamous cell carcinoma: Metastatic squamous cell carcinoma means that the cell cancer has spread beyond the skin to other parts of the body, such as organs of the body. Metastatic squamous cell carcinoma even can spread to mouth, esophagus, bladder, prostate, lungs and reproductive organ.
Causes of squamous cell carcinoma
Exposure to ultraviolet radiation is the high risk of forming squamous cell carcinoma, including UV radiation from sunlight outdoor, tanning lamps and tanning beds indoor. Because over UV radiation will cause mutations in DNA which instruct cells what to do. The mutations and changes of DNA instruct squamous cell to grow multiple quickly. This develops too many uncontrollable squamous cells that break away and spread to other parts of the body. Except for UV radiation, there are other potential factors which cause the development of squamous cell carcinoma such as: a family history, human papillomavirus (HPV) infection, chemical and radiation exposure, smoking and tobacco use, chronic skin inflammation and injury, low immune system, etc.
Dermoscopy in the examination of squamous cell carcinoma
Dermoscopy is a kind of aiding device that helps the detection and diagnosis for dermatologists, by powerful illumination and super magnification. It allows more details of structures, patterns and vessels of epidermis and dermis of the skin that are invisible for naked eyes. According to the typical dermatoscopic features of squamous cell carcinoma, it is clear and precise to identify squamous cell carcinoma from other skin cancers.
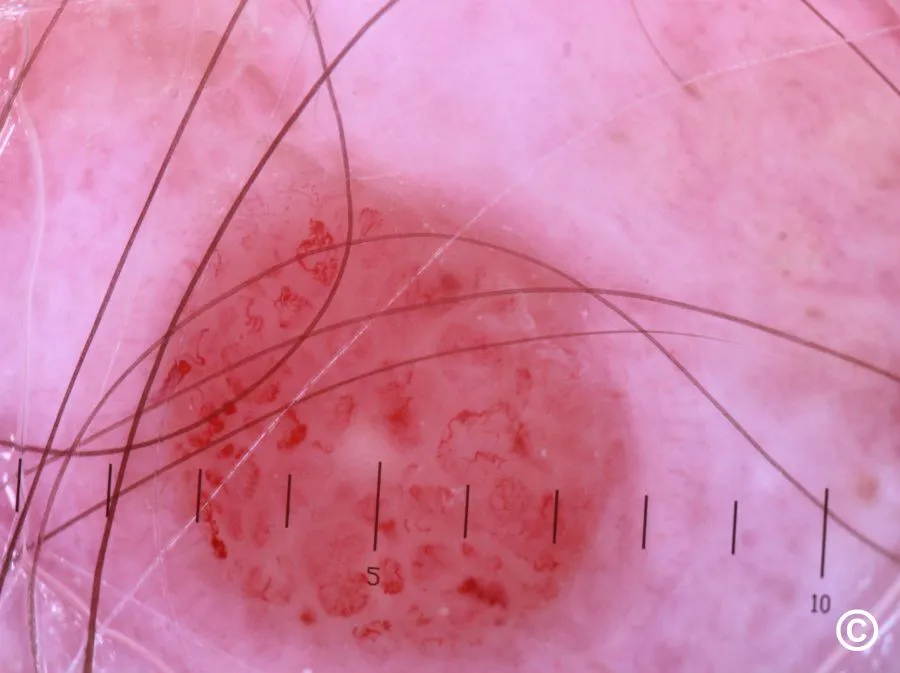
Dermoscopic features of squamous cell carcinoma
Under the use of dermoscopy, skin doctors can observe specific features of squamous cell carcinoma, so that skin doctors can tell and diagnose it more conveniently and clearly, then make a proper treatment schedule for the patients for better cure. There are several specific features of dermoscopic for squamous cell carcinoma including:
Border: Squamous cell carcinoma is usually with irregular and fuzzy border.
Vascular structure: blood spots are very often presented. Blood vessels usually appear in an irregular shape and direction, sometimes in a reticular, radial, punctate, or globular vascular pattern.
White circles: White circles and white undefined areas or white structureless areas
Structure: The structure of squamous cell carcinoma is usually nodular, crusted, or scaly.
Color: Colors of squamous cell carcinoma are usually hazel, brown or black, or a diffuse blue, pink or red.
Others: Squamous cell carcinoma is often accompanied by keratinization, bleeding, or ulcers.
Dermoscopic features of actinic keratosis and squamous cell carcinoma
Since there are some similar appearances of actinic keratosis and squamous cell carcinoma. But dermoscopy can help a lot to distinguish between actinic keratosis and squamous cell carcinoma. There are the comparisons of special demoscopic of actinic keratosis and squamous cell carcinoma as below:
Structure:
Actinic keratosis: Brown structure-less area, ring-shaped particle structure
Squamous cell carcinoma: White structureless areas, nodular, crusted, or scaly structure
Color:
Actinic keratosis: Color of actinic keratosis changes such as brown or red patches, regular pigmentation, especially hyper pigmentation of hair follicle openings.
Squamous cell carcinoma: Colors of squamous cell carcinoma are usually hazel, brown or black, or a diffuse blue, pink or red.
Distribution:
Actinic keratosis: Actinic keratosis distributes in points, lines, etc.
Squamous cell carcinoma: Vessel structure sometimes is in a reticular, radial, punctate, or globular vascular pattern.
Special points:
Actinic keratosis: Strawberry-like pattern, a fine network of thin and dark lines, redness or erythema, white or yellowishe scales
Squamous cell carcinoma: White circles and white undefined areas or white structureless areas, accompany with keratinization, bleeding, or ulcers.

Treatment and management of squamous cell carcinoma
If found early and treated properly, squamous cell carcinoma can get a high cure rate due to its slow growing. There are some commonly treatment methods for squamous cell carcinoma like surgery, radiation therapy and medical treatment.
Prevention strategies for squamous cell carcinoma
To reduce the risk of squamous cell carcinoma, there are some points to be concerned as below:
Limit the sun exposure and other harmful ultraviolet radiation,and avoid to go to outside when the radiation ray is strong.
Use effective sunscreen with at least SPF 30 on the easily exposed areas of skin.
Using umbrellas and wearing protective sunglasses, hat and clothing when go out.
Do self-examination on the skin at least once a month. It is better to use a dermoscopy to do skin examination regularly.
Any suspicious or atypical findings, consult a professional dermatologist for check.
Recommended reading
Dermoscopy of Seborrheic Keratosis – IBOOLO
Seborrheic keratosis is a common skin hyperplasia. It is often mistaken for a disease such as skin cancer because of its appearance that looks like warts, precancerous skin growths, or skin cancer. Dermoscopy of seborrheic keratosis is crucial to identify seborrhei keratosis from other types of skin diseases. What is Seborrheic Keratosis?Seborrheic keratosis...
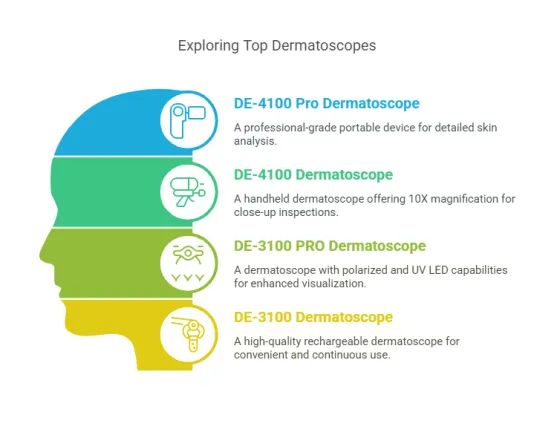
Polarized light dermoscopy: for clearer skin lesion screening - IBOOLO
Polarized light is key in dermoscopy devices for skin lesion screening. IBOOLO-polarized dermatoscopes block surface reflections and clearer observation of subsurface skin anatomy for diagnoses.
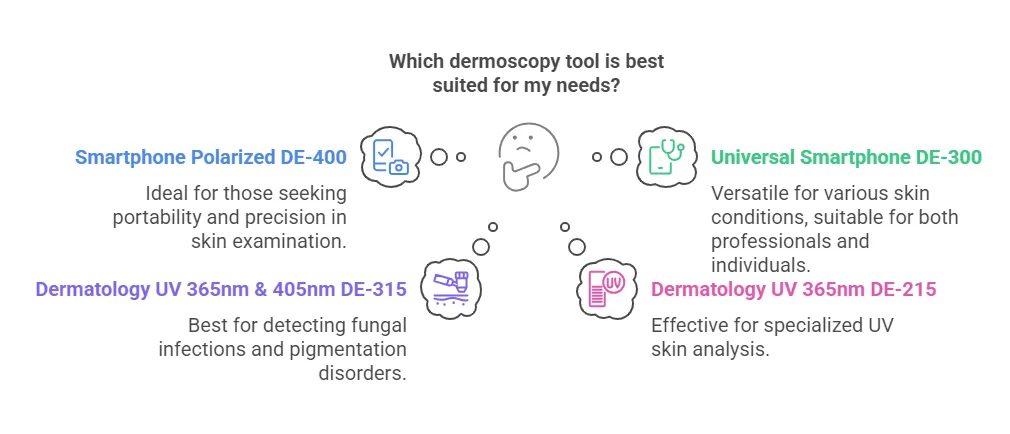
How can dermoscopy images be captured? – IBOOLO
Dermoscopy images can be captured and stored in different ways, such as: • Using a smartphone or tablet with dermoscopic adapter, which consisted in the package.• Using a digital camera with dermoscopic adapter, there’s 49mm screw size camera adapter available to order now. Compatible phone/tablet models:All iPhone models, 95% Android phones, 90% tablet. For...