Article
Dermoscopy of Pigmented Basal Cell Carcinoma
Pigmented basal cell carcinoma refers to a subtype of basal cell carcinoma characterized by the presence of significant amounts of melanin within the tumor and in the surrounding stromal melanophages. It is an uncommon variant of BCC, with a lower incidence rate and usually presents as pigmentation at the site of lesion. PBCC may present…
Pigmented Basal Cell Carcinoma Dermoscopy: Early Detection & Diagnosis
Master the dermoscopic features of pigmented basal cell carcinoma (BCC) for early detection. Learn about key indicators like arborizing vessels, irregular pigmentation, and ulceration. Discover how dermoscopy enhances diagnostic accuracy and improves patient outcomes.
Mastering Pigmented Basal Cell Carcinoma Detection: A Comprehensive Guide to Dermoscopy
Dive into the world of dermoscopy and learn how to identify and manage pigmented basal cell carcinoma (BCC) with precision. This guide explores the key dermoscopic features of pigmented BCC, optimal equipment selection, and step-by-step techniques for accurate diagnosis. Whether you're a clinician or a patient, understanding these principles can significantly enhance early detection and improve outcomes.
What is Pigmented Basal Cell Carcinoma: Dermoscopic Definition and Criteria
Pigmented basal cell carcinoma (BCC) is a subtype of basal cell carcinoma, the most common type of skin cancer. In dermoscopy, what defines it? Pigmented BCC typically shows a combination of characteristic features. One key criterion is the presence of pigmented structures. These can include areas of brown, black, or gray pigmentation. The pigmentation may be unevenly distributed, often in a blotchy or patchy pattern.
Another defining feature is the presence of arborizing telangiectasias. Why are these important? Arborizing telangiectasias are dilated blood vessels that resemble the branches of a tree. In pigmented BCC, they are commonly seen and can be a strong indicator of the condition. Additionally, ulceration or erosion may be present in some cases. When a lesion shows a combination of pigmentation, arborizing telangiectasias, and possible ulceration, it is more likely to be pigmented BCC.
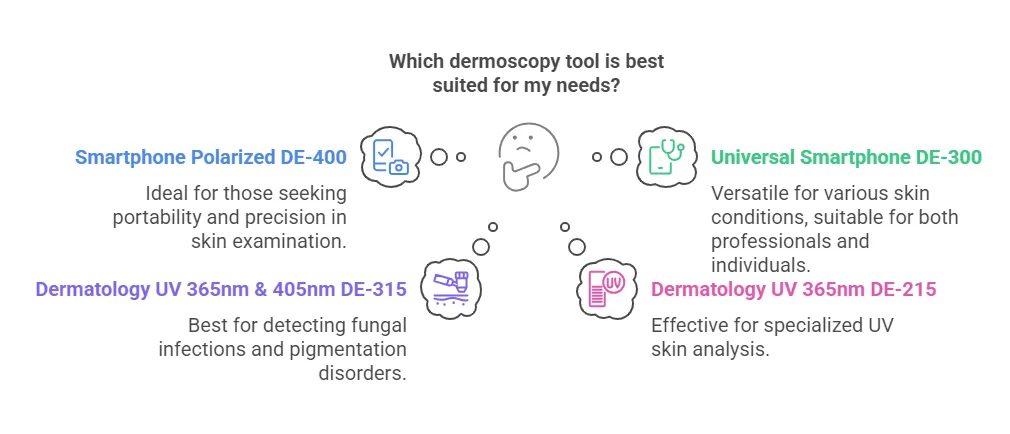
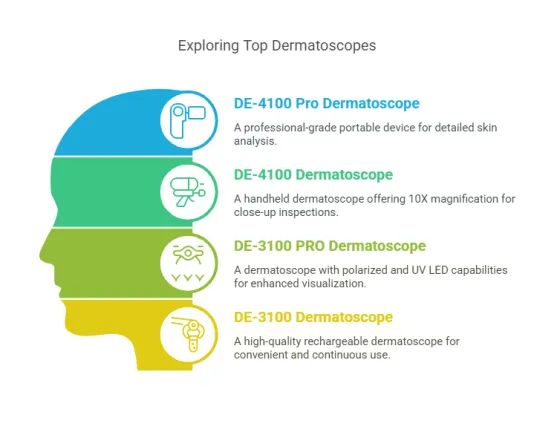
What is the Structure of Dermoscopes Optimal for Pigmented BCC Visualization?
For optimal visualization of pigmented BCC, the structure of the dermoscope matters. A high - quality optical system is fundamental. Why is this crucial? A top - notch optical system, with lenses that offer excellent resolution and contrast, allows dermatologists to clearly see the fine details of pigmented BCC features. Look for dermoscopes with lenses that can minimize chromatic aberration. This ensures that the colors of the pigmented areas and the blood vessels are accurately represented, making it easier to identify the characteristic features of pigmented BCC.
Illumination features also play a critical role. How does illumination impact visualization? Dermoscopes with variable illumination options, such as switchable polarized and non - polarized light, are highly beneficial. Polarized light can reduce surface glare, which is especially useful when trying to visualize the pigmented structures and the underlying arborizing telangiectasias. Adjustable illumination intensity is another advantage. It enables customization based on the patient's skin type and the specific characteristics of the pigmented BCC lesion. For example, in patients with darker skin, higher illumination intensity may be required to penetrate the increased pigmentation and clearly see the features of the pigmented BCC.
Magnification flexibility is an important aspect as well. What magnification range is ideal? A dermoscope that offers a magnification range from around 10x to 40x is often preferred. Lower magnifications, around 10x, can be used for a broad overview of the lesion, allowing the dermatologist to assess its size and general shape. Higher magnifications, up to 40x, are useful for a detailed examination of the pigmented areas, the arborizing telangiectasias, and any other subtle features, which can be crucial for accurate diagnosis.
How to Follow a Clinical Workflow for Dermoscopic Examination of Suspected Pigmented BCC?
When conducting a dermoscopic examination for suspected pigmented BCC, a well - defined clinical workflow is essential. Step by step:
Initial Patient Assessment:
First, obtain a detailed patient history. Why is this important? Information about the patient's age, sun exposure history, family history of skin cancer, and any changes in the skin lesion over time can provide valuable context. For example, a patient with a long - term history of excessive sun exposure and a newly changing pigmented lesion may be at higher risk of pigmented BCC.
Gross Visual Inspection:
Before using the dermoscope, visually examine the suspected lesion. Look for characteristics such as size, shape, color, and the presence of any ulceration or bleeding. This initial inspection can give an idea of whether further investigation with dermoscopy is warranted. A lesion that appears irregular in shape, has a mix of colors, and shows signs of ulceration is more likely to be a concern.
Dermoscopic Examination:
Gently place the dermoscope on the skin surface over the lesion. Adjust the focus and illumination settings according to the guidelines for optimal pigmented BCC visualization. Look carefully for the characteristic features of pigmented BCC, such as pigmented areas, arborizing telangiectasias, and any signs of ulceration. If any of these features are present, note their location, extent, and any associated characteristics within the lesion.
How Do Dermoscopy Working Principles Reveal Pigmented BCC Features?
Dermoscopy works on several principles to reveal the features of pigmented BCC. One of the main principles is the interaction of light with the skin. When light is shone on the skin through the dermoscope, it is absorbed, scattered, and reflected differently by various skin structures. In pigmented BCC, the pigmented areas absorb more light, which is why they appear darker. The arborizing telangiectasias, being dilated blood vessels, reflect light in a characteristic pattern that can be visualized.
For example, in non - polarized light dermoscopy, the pigmented areas may stand out as darker regions, while the arborizing telangiectasias may appear as thin, branching lines. In polarized light dermoscopy, the reduction of surface reflections allows for a better view of the underlying structures. This can make the pigmented areas and the arborizing telangiectasias more distinct, as the light can penetrate deeper into the skin layers and interact with these structures more effectively.
Another principle is magnification. Why is magnification important? By magnifying the skin surface, dermoscopy reveals the fine details of the pigmented BCC features. This magnification enables dermatologists to identify the subtle differences in the pigmentation pattern, the thickness and distribution of the arborizing telangiectasias, and any other minute details that can be crucial for accurate diagnosis.
What is the Proper Technique for Comprehensive Dermoscopic Evaluation of Pigmented BCC?
To perform a comprehensive dermoscopic evaluation of pigmented BCC, several techniques should be followed. First, ensure a proper skin - dermoscope contact. How do you achieve this? Gently place the dermoscope on the skin surface without applying too much pressure. Applying excessive pressure can distort the skin and affect the appearance of the pigmented BCC features.
Adjust the focus carefully. Why is focusing important? A clear focus is essential to accurately identify the subtle features of pigmented BCC, such as the fine branches of the arborizing telangiectasias and the details of the pigmented areas. Start with a low magnification and gradually increase it while adjusting the focus until the skin structures are clearly visible.
Pay attention to the illumination settings. What should you do with illumination? As mentioned earlier, for better visualization of pigmented BCC, use the appropriate type of light (polarized or non - polarized) and adjust the intensity. If the light is too bright or too dim, it can make it difficult to see the features clearly.
Finally, scan the entire lesion systematically. In a list format:
Start from one edge of the lesion.
Move the dermoscope slowly across the lesion, ensuring that every part of the lesion is examined.
Look for any areas that show the characteristic features of pigmented BCC, such as the presence of pigmented blotches, arborizing telangiectasias, or signs of ulceration.
Note the location, extent, and any associated features of these areas within the lesion.
What Are the Clinical Applications of Dermoscopy in Different Subtypes of Pigmented BCC?
Dermoscopy serves various clinical purposes for different subtypes of pigmented basal cell carcinoma (BCC). In nodular pigmented BCC, dermoscopy can help in precisely determining the tumor's border. How? By visualizing the characteristic arborizing telangiectasias and pigmented areas, dermatologists can accurately demarcate the extent of the nodule. This is crucial for planning surgical excision, as a clear understanding of the tumor's boundaries ensures complete removal, reducing the risk of recurrence.
For superficial pigmented BCC, dermoscopy can identify subtle features like the presence of a fine network - like pattern. Why is this important? This pattern can help distinguish superficial pigmented BCC from other similar - looking skin lesions. It also aids in monitoring the spread of the lesion over time. Regular dermoscopic examinations can detect any changes in the network pattern, such as its expansion or the appearance of new pigmented areas, guiding decisions on the need for more aggressive treatment.
In morpheaform pigmented BCC, dermoscopy may reveal areas of white - scar - like appearance along with pigmentation. How does this assist clinically? Recognizing these features can help in differentiating morpheaform BCC from other skin conditions. It also provides information about the depth and invasiveness of the tumor, which is valuable for choosing the most appropriate treatment modality, such as Mohs micrographic surgery for more invasive lesions.
How Accurate Is the Diagnostic Accuracy of Dermoscopy in Pigmented BCC vs. Melanoma?
Dermoscopy is a valuable tool for differentiating pigmented BCC from melanoma, but its accuracy depends on several factors. Pigmented BCC often shows characteristic features like arborizing telangiectasias and pigmented globules in a specific pattern. In contrast, melanoma typically presents with asymmetry, border irregularity, color variegation, and a different pattern of pigment network. However, there can be overlapping features, which may reduce the diagnostic accuracy.
To improve accuracy, dermatologists use a combination of dermoscopic features and clinical information. What kind of clinical information? Patient history, such as age, sun exposure, and family history of skin cancer, can provide context. For example, a younger patient with a pigmented lesion is more likely to have a benign or less aggressive condition like pigmented BCC, while an older patient with a rapidly changing, irregularly pigmented lesion may be at higher risk of melanoma. Additionally, experienced dermatologists may use specific algorithms or scoring systems that take into account multiple dermoscopic features to increase the diagnostic accuracy in differentiating between the two.
What Are the Key Features to Look for in Dermoscopes for Optimal Pigmented BCC Visualization?
When seeking a dermoscope for optimal pigmented BCC visualization, several key features should be considered. A high - resolution optical system is essential. Why? It allows for clear visualization of the fine details of pigmented BCC, such as the delicate branches of arborizing telangiectasias and the texture of pigmented areas. Look for dermoscopes with lenses that offer excellent contrast, as this helps in differentiating between different structures within the lesion.
Illumination features play a crucial role. How does illumination impact visualization? Dermoscopes with variable illumination options, like switchable polarized and non - polarized light, are highly beneficial. Polarized light reduces surface reflections, which is especially useful for visualizing the underlying pigmented structures and blood vessels in pigmented BCC. Adjustable illumination intensity is also important. It enables customization based on the patient's skin type and the specific characteristics of the lesion. For instance, in patients with darker skin, higher illumination intensity may be required to penetrate the increased pigmentation and clearly see the features of pigmented BCC.
Magnification flexibility is another important aspect. What magnification range is ideal? A dermoscope that offers a magnification range from approximately 10x to 40x is often preferred. Lower magnifications, around 10x, are useful for getting an overall view of the lesion, allowing the dermatologist to assess its size and general shape. Higher magnifications, up to 40x, enable a detailed examination of the fine features of pigmented BCC, such as the thickness of the arborizing telangiectasias and the distribution of pigment within the globules.
What Are the Quality Standards in Dermoscopic Evaluation of Pigmented Basal Cell Carcinoma?
Quality standards in the dermoscopic evaluation of pigmented BCC are vital for reliable diagnoses. Standardized image acquisition is the first step. How should this be carried out? Dermoscopists should follow a strict protocol for placing the dermoscope on the skin. They need to ensure consistent pressure and contact across all examinations. This consistency is crucial because inconsistent pressure can distort the skin surface, altering the appearance of the pigmented BCC features. The images should be of high resolution, with proper focus and exposure. High - resolution images capture the fine details of the arborizing telangiectasias, pigmented areas, and any other relevant features, while correct focus and exposure ensure that these features are clearly visible.
Accurate interpretation of dermoscopic findings is another key quality standard. Dermoscopists must be well - trained in recognizing the characteristic features of pigmented BCC. In a list format:
They need to be able to differentiate between true pigmented BCC features and artifacts. Artifacts can arise from factors like improper dermoscope placement or dirt on the skin surface, and misinterpreting them as pigmented BCC features can lead to incorrect diagnoses.
Understanding the relationship between different dermoscopic features and the aggressiveness of pigmented BCC is essential. For example, the presence of extensive ulceration or a large number of abnormal blood vessels may indicate a more aggressive form of the disease.
Participating in continuing education programs and quality assurance initiatives helps dermoscopists stay updated on the latest research and best practices related to pigmented BCC evaluation.
Documentation of dermoscopic findings also adheres to quality standards. All relevant information, such as the exact location of the lesion on the body, the extent and distribution of pigmented areas, the presence and characteristics of arborizing telangiectasias, and any associated features like ulceration or scar - like areas, should be clearly and comprehensively recorded. This detailed documentation serves as a reference for future consultations and for tracking the evolution of the patient's condition over time.
What Precautions Should Be Taken When Interpreting Pigmented BCC Patterns in Different Skin Types?
Interpretation of pigmented BCC patterns requires special precautions when dealing with different skin types. In darker - skinned individuals, the natural pigmentation can pose challenges. How can these be overcome? Dermatologists must be well - versed in the normal pigmentation variations specific to different ethnic groups. For example, in darker - skinned patients, there may be increased pigmentation around hair follicles or in certain skin areas, which can be mistaken for pigmented BCC features. To avoid misinterpretation, appropriate illumination settings should be used. Increasing the intensity of polarized light can help to better differentiate between normal pigmentation and the pigmented areas associated with BCC. By reducing surface reflections and enhancing the contrast within the skin layers, the true nature of the pigmentation pattern becomes more apparent.
In lighter - skinned patients, the pigmented BCC features may be more difficult to detect due to lower contrast. What steps can be taken? Dermoscopists need to be meticulous in adjusting the magnification and focus. Since the features of pigmented BCC may be more subtle in lighter skin, precise adjustments are necessary to bring them into view. Additionally, if the dermoscope is equipped with image enhancement features, such as digital contrast adjustment or edge enhancement, these can be employed to improve the visibility of the arborizing telangiectasias and pigmented areas. It's also important to consider the patient's overall skin condition. Sun damage, for instance, can alter the skin's appearance and potentially affect the visibility and interpretation of pigmented BCC patterns. By taking these factors into account, dermatologists can more accurately interpret pigmented BCC patterns across all skin types.
What: Maintenance of Dermoscopic Equipment for Precise Pigmented Lesion Assessment
Dermoscopy is a crucial tool in the diagnosis and management of pigmented lesions, including pigmented basal cell carcinoma (BCC). However, the accuracy of dermoscopic assessments heavily relies on the proper functioning of the equipment. Here are some essential steps to maintain dermoscopic devices for precise assessments:
Regular Cleaning: Ensure the lens and contact surfaces are free from dirt and smudges. Use a soft, lint-free cloth and a mild cleaning solution to gently wipe the lens.
Calibration Checks: Periodically check the calibration of the device to ensure accurate magnification and lighting. Follow the manufacturer's guidelines for calibration procedures.
Software Updates: Keep the dermoscopy software up to date to benefit from the latest features and improvements in image analysis.
Training and Familiarization: Ensure that all users are well-trained and familiar with the device's operation. This includes understanding how to adjust settings for different skin types and lesion characteristics.
Proper maintenance not only extends the lifespan of dermoscopic equipment but also enhances the reliability of assessments, ultimately contributing to better patient outcomes.
Why: Digital Dermoscopy for Tracking Pigmented BCC Treatment Response
Digital dermoscopy has revolutionized the way we monitor the response of pigmented basal cell carcinoma to treatment. Here are several reasons why digital dermoscopy is essential:
Accurate Documentation: Digital dermoscopy allows for precise and consistent documentation of lesions over time. High-resolution images can be stored and compared easily, providing a clear visual record of changes.
Quantitative Analysis: Advanced digital dermoscopy systems offer tools for quantitative analysis, such as measuring lesion size, color changes, and structural alterations. This helps in objectively assessing treatment efficacy.
Enhanced Communication: Digital images can be shared easily among healthcare providers, facilitating better collaboration and continuity of care. This is particularly important in multidisciplinary teams managing complex cases.
Patient Education: Visual documentation helps in educating patients about their condition and the progress of treatment. This can improve patient compliance and satisfaction.
By leveraging digital dermoscopy, clinicians can provide more personalized and effective care for patients with pigmented BCC.
How: Dermoscopic Patterns Specific to Pigmented Basal Cell Carcinoma: A Visual Guide
Identifying dermoscopic patterns specific to pigmented basal cell carcinoma is crucial for early and accurate diagnosis. Here are some key patterns to look for:
Irregular Pigmentation: Pigmented BCC often presents with irregular pigmentation, including areas of dark brown or black. This is different from the more uniform pigmentation seen in benign lesions.
Structureless Areas: The presence of structureless areas, especially with a bluish-gray hue, is a common feature. This is due to the dense cellular arrangement in BCC.
Irregular Vessels: Pay attention to irregular, arborizing, or polymorphous vessels. These can be a red flag for malignancy.
Peripheral Pigmentation: Pigmented BCC may show peripheral pigmentation with a "string of pearls" appearance, where pigmented dots or globules are arranged along the periphery of the lesion.
Step by Step: Identifying Suspicious Patterns
1. Initial Assessment: Begin with a macroscopic examination of the lesion.
2. Dermoscopic Examination: Use a polarized or non-polarized dermoscope to examine the lesion closely.
3. Pattern Recognition: Look for the specific patterns mentioned above.
4. Comparison with Normals: Compare the findings with known benign patterns to identify deviations.
5. Consultation: If unsure, consult with a dermatologist or use dermoscopic atlases for reference.
Being familiar with these patterns can significantly improve diagnostic accuracy and lead to early intervention.
Can: Differentiating Pigmented BCC from Other Pigmented Lesions Using Dermoscopy
Distinguishing pigmented basal cell carcinoma from other pigmented lesions can be challenging, but dermoscopy offers valuable clues. Here are some tips to help differentiate:
Compare with Benign Lesions: Benign pigmented lesions, such as melanocytic nevi, typically show regular pigmentation patterns, symmetric structures, and uniform vessels. In contrast, pigmented BCC often presents with asymmetry and irregular features.
Look for Specific Clues: As mentioned earlier, the presence of structureless areas, irregular vessels, and peripheral pigmentation are more suggestive of BCC.
Use the ABCD Rule: While primarily used for melanoma, the ABCD rule (Asymmetry, Border irregularity, Color variation, and Diameter) can also be applied to pigmented BCC. Lesions with these features should raise suspicion.
Consider Clinical Context: Pigmented BCC often occurs in sun-exposed areas, such as the face and neck. Combine dermoscopic findings with clinical context for a more accurate diagnosis.
Step by Step: Differential Diagnosis
1. Initial Screening: Use dermoscopy to identify suspicious features.
2. Rule Out Benign Lesions: Compare with typical patterns of benign lesions.
3. Confirm Suspicious Patterns: Look for specific dermoscopic patterns associated with BCC.
4. Consultation: If uncertain, seek a second opinion or perform a biopsy for confirmation.
Effective differentiation using dermoscopy can prevent unnecessary biopsies and ensure timely treatment for pigmented BCC.
Does: The Role of Dermoscopy in Early Detection of Pigmented Basal Cell Carcinoma
Early detection of pigmented basal cell carcinoma is critical for effective treatment and better patient outcomes. Dermoscopy plays a pivotal role in this process. Here's how:
Enhanced Visualization: Dermoscopy allows for a detailed examination of skin lesions, revealing features not visible to the naked eye. This includes subtle pigmentation changes and structural alterations.
Improved Diagnostic Accuracy: By identifying specific dermoscopic patterns, clinicians can differentiate pigmented BCC from benign lesions more accurately.
Non-Invasive Screening: Dermoscopy is a non-invasive technique, making it suitable for routine screening of high-risk patients or those with multiple pigmented lesions.
Early Intervention: Early detection through dermoscopy enables timely intervention, often with less invasive treatments and better cosmetic outcomes.
Step by Step: Implementing Dermoscopy for Early Detection
1. Patient Screening: Identify high-risk patients, such as those with a history of skin cancer or significant sun exposure.
2. Regular Examinations: Perform routine dermoscopic examinations of pigmented lesions.
3. Pattern Recognition: Train clinicians to recognize specific dermoscopic patterns associated with BCC.
4. Follow-Up and Monitoring: Use digital dermoscopy to track changes in suspicious lesions over time.
This article provides an in-depth look at the dermoscopic evaluation of pigmented basal cell carcinoma (BCC), the most common subtype of skin cancer. We discuss the characteristic features of pigmented BCC, including irregular pigmentation, arborizing telangiectasias, and ulceration, and how these can be identified using dermoscopy. The guide covers essential aspects such as the optimal structure of dermoscopes, clinical workflows for examination, and the importance of maintaining equipment. Additionally, we explore how dermoscopy can differentiate pigmented BCC from other lesions and its role in early detection and treatment monitoring. By following the principles outlined in this article, clinicians can improve diagnostic accuracy and provide better care for patients with pigmented BCC.
Recommended reading
Buy the best dermatoscopes for skin screening and analysis - IBOOLO
IBOOLO offers the best professional dermatoscopes available for purchase buy online. Shop a range of digital dermatoscopes for dermoscopy, mole screening, clinical analyses, and more.
How can I clean my dermoscopy after usage? – IBOOLO
Cleaning your dermoscopy after usage is important to prevent cross-contamination and infection. The cleaning method may vary depending on the type and model of your dermoscopy, so you should always follow the manufacturer’s instructions. However, some general steps are: • Turn off and disconnect your dermoscopy from any power source or device. • Wipe off...
Our China Portable Suppliers & Manufacturers Easy to Carry Dermoscopy Price - IBOOLO
Our China suppliers & manufacturers utilizes durable composites and expert craftsmanship to manufacture portable dermoscopy price capable of withstanding rugged mobile use without compromising image quality.
Pigmented basal cell carcinoma refers to a subtype of basal cell carcinoma characterized by the presence of significant amounts of melanin within the tumor and in the surrounding stromal melanophages. It is an uncommon variant of BCC, with a lower incidence rate and usually presents as pigmentation at the site of lesion. PBCC may present initially as only mild pigmentour alterations and slight skin changes, which could possibly remain unrecognizable. Because dermoscopy is extremely sensitive, it can find these subtle changes and thus allows to detect this earlier.
What is pigmented basal cell carcinoma?
Epidemiologically, pigmented basal cell carcinoma occurs more frequently with increasing age. In addition, risk factors involved in the PBCC pathogenesis include chronic malady of sun exposer (sunbathing), presence of ultraviolet radiation and ionizing Radiation, Chemical contamination; outside stimuli are included with genetic factor. PBCC is the most challenging because early diagnosis and treatment are critical. Although the disease had a low-grade malignant potential, untreated PBCC could cause much harm to its carrier.
The most distinct difference between pigmented basal cell carcinoma and other forms of basal cellular carcinomas (such as nodular ulcerative type, superficial type) is the prominent hyperpigmentation of the lesions in contrast to those that show mostly different colors rather than black. Compared with non-pigmented basal cell carcinoma, the incidence of pigmented BCC is low.

Advantages of dermoscopy in the diagnosis of pigmented skin lesions
The basic principle of dermoscopy is the use of optical magnification to avoid reflected light from then surface and provide enlargement on fine structures at the skin surface, allowing a deeper look further beyond stratum corneum or even in superficial dermis. Dermoscopy should be done under the supervision of a dermatologist. The skin in the lesion area should be relatively dry before examination, and lubricants or ointments are not applied.
This technique visualizes skin structures that are not easily observed by the naked eye, including a detailed dermatoscopic view of pigment networks and vascular patterns among other important diagnostic landmarks to aid in early diagnosis from melanomas and pigmented basal cell carcinoma. Moreover, dermoscopy is a non-destructive and elegant process that involves no pain or harm to the patient. Dermoscopy is a simple, quick and inexpensive method as compared to other screening methods.
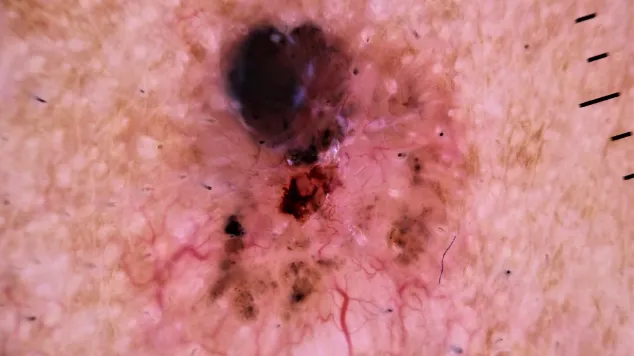
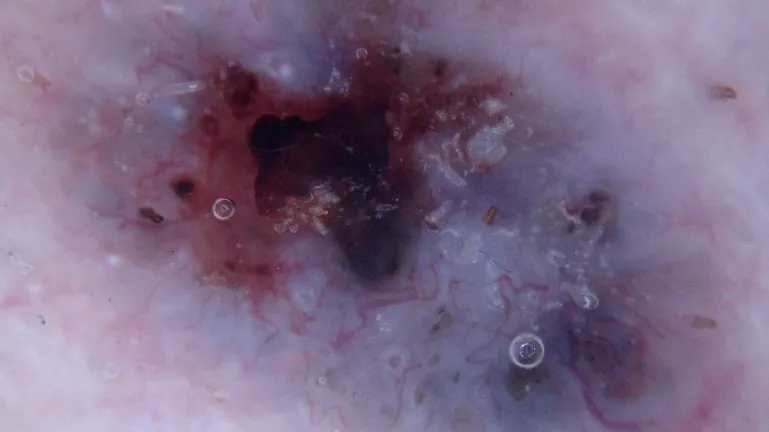
Dermoscopic features of pigmented basal cell carcinoma
Blue-gray globules: dermoscope might sometimes show large, round or oval structures which appear to be filled with melanin reflected as bluish-grey.
Dendritic blood vessels: a dermoscopic hallmark of basal cell carcinoma, also seen in pigmented BCC. This pattern is dendritic and originates from a central point, making it very distinctive.
Pigmentation network: PBCC often shows a lack of a typical pigmentation network; instead, it may appear as an unstructured or foliated area around the lesion.
Differences between pigmented basal cell carcinoma and other pigmented skin lesions
Dermoscopy allows the visualization of features crucial to distinguishing PBCC from other pigmented lesions
(1). Melanoma.
Appearance: The lesion is asymmetrical with irregular borders and many colors (brown, black, blue, red ).
Dermoscopy: Atypical pigmentation network, irregular streaking with blue-white veil.
Difference: PBCC typically shows blue-gray blobs, dendritic vessels surrounding usual pigment network
(2). Blue nevus.
Appearance: A unique lesion that is blue or black
Dermoscopy: Uniform blue pigmentation without any structure
Distinction: PBCC has additional features such as dendritic vessels and blue-gray ovoid nests
(3). Solar Lentigo.
Appearance:Brown macules that are flat and often found in sun-exposed sites
Dermoscopy: A fine mesh pattern of uniform pigmentation.
Difference: PBCC demonstrates a more complex arrangement of blue-gray globules and dendritic blood vessels
Interpretation difficulties and common pitfalls in dermoscopic images of pigmented basal cell carcinoma
The resultant dermoscopic image of PBCC generally shows a complex structure with various types of blue-grey blobs and dendritic blood vessels, which demand very-rich experience as well as expertise in the identification and interpretation process. Moreover, dermoscopic features of PBCC may resemble some benign lesions like blue nevi and pigmented nevus which should be accurately differentiated in reading.
During interpretation of dermoscopic images, some doctors may focus too much on a single criterion (e.g., blue-gray blobs) and ignore other clinical data or notable features observed through polarisation analysis. Moreover, pigmented basal cell carcinoma also presents as a black papule or nodule and its dermoscopic image resembles that of melanoma. Consequently, sometimes a biopsy is done to differentiate pigmented basal cell carcinoma from melanoma.
A clinical case of pigmented basal cell carcinoma
Case Presentation
Patient: 65-year-old male with a long history of sun exposure and pigmented lesion on left cheek. It has been slowly growing larger for the last 12 months.
Examination: 1.5 cm ill-defined dark plaque with a sclerotic surface
Dermoscopic examination:
(1) A bluish or grayhill to brown net is observed which has a different color and intensity in the various areas of the plaque.
(2) Multiple blue-gray spherules irregularly arranged and surrounded by normal skin
(3) Maple-like appearance at edges of the plaque with tiny dendritic blood vessels distributed in marginal areas.
Diagnostic process:
Preliminary Diagnosis: Clinical and dermatoscopic features were consistent with the diagnosis of pigmented basal cell carcinoma.
Further Examination: A biopsy from the margin of plaque was obtained under local anesthesia.
Histopathological Results: Pathological sections showed the presence of a tumor mass in the dermis composed of basal-like cells. Melanocytes were seen in the tumor parenchyma and melanophagocytes were seen in the interstitium, consistent with pigmented basal cell carcinoma.
Diagnosis:
He was eventually diagnosed with pigmented basal cell carcinoma.
Association between dermoscopic and histologic features
Pigmented lesions: Dermoscopic features of pigmented lesions often reflect the proliferation, distribution and arrangement of melanocytes within the lesion, as well as the morphology and density of blood vessels.
Non-pigmented lesions: The dermoscopic features of non-pigmented lesions are often associated with changes in cellular components such as keratinocytes and fibroblasts within the lesion.
Vascular structure: Dermoscopic features of vascular structure are often consistent with histopathologic changes in vascular morphology and density. For example, in inflammatory dermatoses, the dermoscopic vascular structure may exhibit features such as dilatation and congestion, which are consistent with a histopathologic vascular inflammatory response.