Article
Dermoscopy of Lichenoid Keratosis
Lichenoid Keratosis occurs in middle-aged and elderly people, especially in sun-exposed areas such as the head, face, neck and dorsum of the hands. It is characterized by a wide variety of clinical manifestations, which can be easily confused with other similar lesions such as seborrheic keratosis, lichen planus and chronic lichenoid keratosis, leading to misdiagnosis…
Lichenoid Keratosis occurs in middle-aged and elderly people, especially in sun-exposed areas such as the head, face, neck and dorsum of the hands. It is characterized by a wide variety of clinical manifestations, which can be easily confused with other similar lesions such as seborrheic keratosis, lichen planus and chronic lichenoid keratosis, leading to misdiagnosis and underdiagnosis. Dermoscopy can clearly show the pigment granules in lichenoid keratosis lesions, which are diffusely distributed and coarse, a feature that helps to differentiate lichenoid keratosis from other similar lesions.
What Is Lichenoid Keratosis?
Lichenoid keratosis, also known as benign lichenoid keratosis or isolated lichen planus keratosis, is a benign keratotic skin disease with moss-like histologic changes. Its etiology is unclear and may be related to a number of factors, including genetic factors, abnormalities of the immune system, viral infections, and chronic ultraviolet exposure. Due to the relative infrequency of lichenoid keratosis, specific prevalence data are difficult to obtain, but the incidence is generally considered to be low.
Lichenoid keratosis presents as single or multiple well-demarcated keratotic plaques, mostly red to dark red in color, some with uneven pigmentation. The surface of the lesions may be smooth or have wart-like protrusions, varying in size and usually ranging from 5 to 20 mm in diameter.

Clinical Distinction between Lichenoid Keratosis and Lichen Planopilaris
Lichenoid Keratosis: the color is mostly red to dark red, some have uneven pigmentation. The main manifestations are epidermal hyperkeratosis, thickening of the stratum spinosum and other moss-like changes.
Lichen Planopilaris: its lesions are mainly distributed around hair follicles, forming follicular papules or plaques, often accompanied by abnormalities and destruction of hair follicle structure.
Basics of Dermoscopy
Dermoscopes are mainly composed of a lens, a mirror body, and an adjustment knob. Before observing with a dermatoscope, clean the skin area to be examined. Then adjust the magnification and focusing distance of the dermatoscope as needed. Finally, place the dermatoscope on the skin area to be observed and observe the surface of the skin and the structure of the lower layers of the skin from different angles.
The high-resolution magnified images of dermoscopy can help doctors distinguish benign tumors from malignant skin cancer lesions. Moreover, dermoscopy is a non-invasive, visualized diagnostic tool for dermatological diseases, which does not traumatize the patient’s skin, reduces the patient’s nervousness and improves the patient’s cooperation.
Dermoscopic Features of Lichenoid Keratosis
Lichenoid keratosis are often seen dermoscopically as pigment granules, which may be bluish-gray, brownish-red, or other colors. The pigment granules are diffusely distributed or may be focally distributed. They are usually less than 1 cm in diameter, flat or slightly elevated, and tend to have a smooth surface but occasionally scaly or warty. The lesions usually progress from an inflammatory phase (where some pink discoloration may occur) to a hyperpigmented phase (where the color of the lesion becomes grayish brown).

Lichenoid Keratosis and Other Lesions
Lichenoid keratosis, follicular lichenoid moss and malignant melanoma can be well differentiated by using dermoscopy, and the following are key points of their dermoscopic differentiation.
Lichenoid Keratosis usually has regular margins and lesions of various shapes. The pigmentation abnormalities in Lichenoid Keratosis may not be as dramatic as those of Malignant Melanoma, but some patients may still have deepening, hypopigmentation, or uneven pigmentation.
The distinguishing dermoscopic feature of follicular lichenoid moss is follicular involvement, such as hyperkeratosis of follicular openings, perifollicular erythema, or hyperpigmentation. The lesions may be covered with scales and are often associated with hyperkeratosis.
Malignant melanoma often appears dermoscopically as a mixture of colors with uneven distribution. The shape and color distribution of the lesions are often asymmetric and poorly demarcated from the surrounding normal skin.
Can Lichenoid Keratosis Become Cancerous?
Lichenoid Keratosis, a benign keratotic skin disease, does not usually transform into cancer. If the lesions are small and there are no obvious uncomfortable symptoms, they can be observed regularly and left untreated for the time being. If the lesion is large, or has obvious self-conscious symptoms, such as itching, pain, etc., affecting the patient’s daily life, then it can be considered for excision.

Dermoscopically Guided Clinical Decision Making
Utilizing dermoscopic findings for clinical decision-making, including biopsy and treatment selection, is a comprehensive process. When dermoscopic findings show skin lesions with malignant features or a high suspicion of malignancy, biopsy should be considered for definitive diagnosis. The choice of treatment, however, depends largely on the type of dermoscopic lesion. For benign lesions, observation and follow-up, topical medications, and physical therapy can be used for treatment. For malignant skin lesions, comprehensive treatment methods such as surgical excision, chemotherapy and radiotherapy should be chosen according to the severity of the disease.
Clinical Case Studies
Background
A middle-aged woman complained of a brown maculopapular rash on her shoulders for several years, which had recently increased in number and was accompanied by mild itching.
Clinical Examination:
The patient had multiple brown maculopapular rashes on the neck and shoulders, with rough and slightly flaky surfaces.
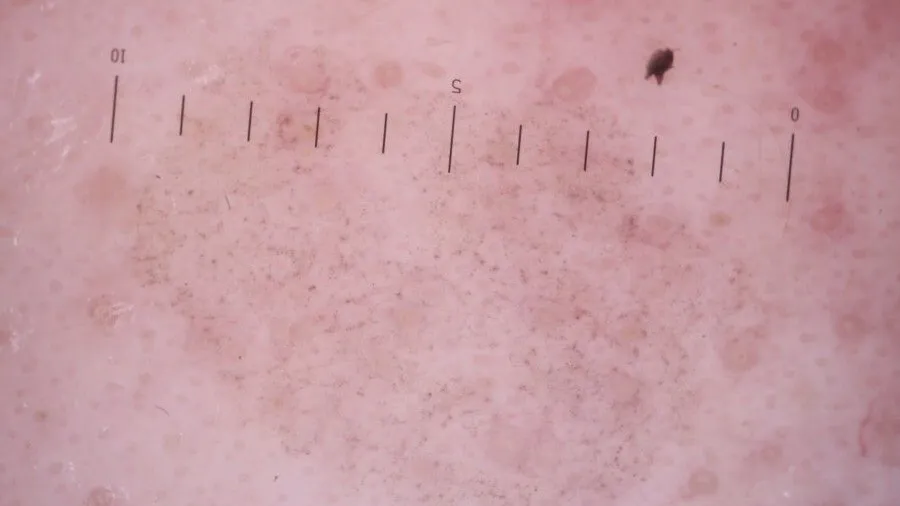
Dermoscopy:
Dermoscopy revealed dense brownish-red pigmented granules on the surface of the lesions, which were diffusely or focally distributed. Worm-eaten changes were seen at the edges of some of the lesions, and hypopigmented areas were seen in the center of the lesions. The surface of the lesions is covered with a thin layer of scales and the skin texture is thickened.
Dermoscopic image interpretation:
Brownish-red pigmented granules help to differentiate between the different types of skin diseases. The lesions are covered with a thin layer of scales, suggesting hyperkeratosis and hypertrophy of the stratum spinosum. Wormy edges are a characteristic manifestation of Lichenoid Keratosis.
Treatment and Management of Lichenoid Keratosis
Topical treatments are one of the main therapeutic options for lichenoid keratosis, aiming to use medications that act directly on the lesions to relieve symptoms and promote skin recovery. Phototherapy uses specific wavelengths of ultraviolet light to irradiate the damaged area to promote hyperpigmentation and cell renewal, which can help improve mossy keratoses.
During the course of treatment, it is important to closely monitor the patient’s response to treatment, which includes observing changes in the lesions, assessing the degree of improvement in symptoms, and noting the presence of adverse reactions. And patients should be provided with appropriate scientific information and education, such as explaining the causes of lichenoid keratosis, instructing patients on how to use topical medications correctly, and encouraging patients to maintain a positive and optimistic mindset. All this is conducive to the recovery of patients.
Diagnostic Procedures for Dermoscopy
First, the patient needs to clean the skin surface to be examined, and the physician conducts a preliminary clinical examination to determine the possible types of diseases. The probe of the dermatoscope is gently applied to the skin surface to be observed, maintaining an appropriate distance. Then adjust the focus, carefully observe the skin lesions, the doctor will be based on their own experience to determine the type of skin disease. Dermoscopy is able to magnify and clearly display the fine structure of the skin surface, helping the physician to more accurately identify the characteristic changes of the skin lesion, thus improving the accuracy of diagnosis.