Article
Dermoscopy of Ink Spot Lentigo
Ink Spot Lentigo, also commonly referred to as reticular black sunspots or ink spot-like pigmented nevi, is a specific type of skin pigmentation lesion. Most Ink Spot Lentigo are benign, with only a very small percentage developing into malignant melanoma. Dermoscopy magnifies the lesion many times over, allowing the doctor to clearly observe Ink Spot…
Ink Spot Lentigo, also commonly referred to as reticular black sunspots or ink spot-like pigmented nevi, is a specific type of skin pigmentation lesion. Most Ink Spot Lentigo are benign, with only a very small percentage developing into malignant melanoma. Dermoscopy magnifies the lesion many times over, allowing the doctor to clearly observe Ink Spot Lentigo’s borders, colour distribution, blood vessel patterns and other subtle features.
What Is Ink Spot Lentigo?
Dark spots on the skin that look like ink can be a sign of a variety of skin problems including, but not limited to, freckles, pigmented moles, and age spots. Therefore, such dark spots cannot simply be equated directly with ink spot freckles.
Ink Spot Lentigo is a darkly pigmented, distinctly irregular spot with reticular or beaded edges, similar to an ink spot on the skin. Its lesions are usually confined to areas of sun-exposed skin, such as the face, neck, and arms. From a medical classification point of view, Ink Spot Lentigo belongs to a type of skin pigmented lesion, specifically classified as a subtype of solar freckle-like nevus.
Dermoscopy in the Detection of Ink Spot Lentigo
Dermoscopy uses optical magnification technology to look at skin details that are invisible to the naked eye. The accuracy of diagnosis of lentigo by dermoscopy doctors is improved as they are able to identify clearly the fine structure and color changes of lentigo ink spot and differentiate it from skin lesions such as melanoma.
Dermoscopy enables imaging of subsurface structures and colors which are not visible to the naked eye. Proper utilization of this skill leads to the detection of melanoma and other skin cancers in the early stages which may result in more effective and earlier treatment. By providing a more detailed examination, dermoscopy can help differentiate between benign and malignant lesions more effectively. This reduces the number of unnecessary biopsies and excisions, minimizing patient anxiety and healthcare costs.
Dermoscopic Features of Ink Spot Lentigo
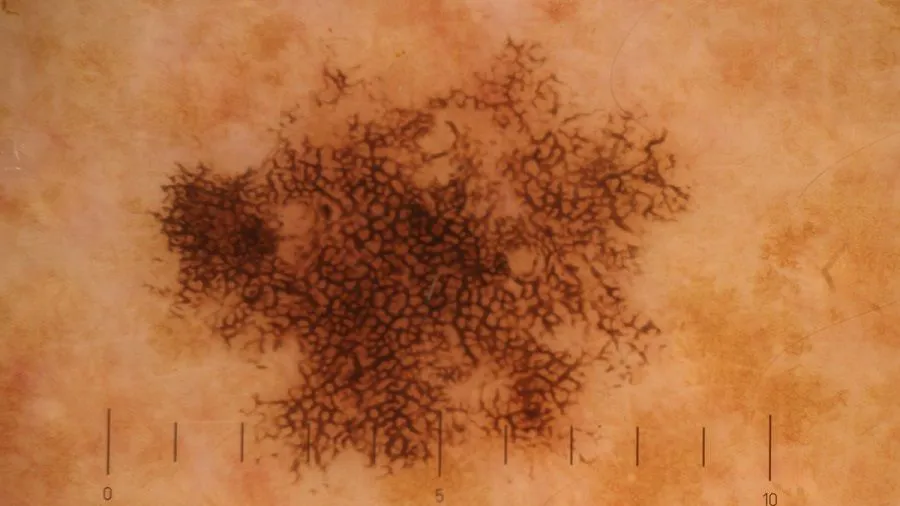
Pigmented Webs: The lesions in question are characterized by a conspicuous black-pigmented net, which under dermoscopy can be said to have a three-dimensional effect. The Iines of the network can be different in thickness.
Pigmented Dots: Within the lesion, there can be small black pigmented dots which are dark.
Irregular Pigment Distribution: The ink spot lentigo pigmentation is also mostly uneven with a mix of black areas and light ones for instance.
Relationship between Ink Spot Lentigo and Malignant Melanoma
Ink spot lentigo is commonly a harmless condition of the skin that is caused by a group of melanocytes in the skin, while malignant melanoma is a very aggressive skin cancer that comes from melanocytes and grows very fast as well as spreads to other parts of the body. Ink spot lentigo rarely progresses to malignant melanoma, which is usually associated with genetic and environmental predispositions.
Malignant melanoma that has been detected in the early stage can be dealt with surgical and some other treatment options easily. Tumours that are detected at a later stage are often very difficult to cure. Early detection and monitoring of precursor lesions of potentially malignant melanoma like “ink spot lentigo” can help to identify the risk of malignancy and provide the necessary treatment in a timely manner. This,in turn, leads to a better patient survival rate.

The Challenge in Identifying Ink Spot Lentigo
Ink spot lentigo is a special type of pigmented skin lesion which distinguishes itself from the commonly known examples of such skin lesions such as freckles and solar lentigines through its unique features such as dark brown to black spots, possible irregular shape. Freckles, on the other hand, are usually found on exposed areas and their colour is significantly affected by sunlight; solar lentigines are the places that are very much exposed to ultraviolet rays and they may increase in number and deepen with age and exposure to ultraviolet rays.
Dermoscopic Image-guided Clinical Management
Patient: Female, 45 years old, presented with a progressive, unevenly pigmented plaque found on the right forearm. The plaque reported by the patient was there for a few years and had recently become more dark and blurred.
Dermoscopy: The dermatoscope revealed black, brown, and gray, which showed the atypical network of reticulation, annularity, or irregular distribution.
Clinical decision-making: Based on the above dermoscopic features, there was a high degree of suspicion that this lesion was an early melanoma or a pigmented skin pre-cancer. Therefore, it was decided to biopsy the patient.
Treatment decision: If the diagnosis is malignant melanoma, surgical excision or chemotherapy is required. If it is a benign lesion but there is a potential risk of malignancy, prophylactic excision or laser treatment may be considered.
Ink Spot Lentigo Treatment Strategy and Management
Laser therapy which is a widely used and very successful method of getting rid of ink spots, freckles, and ink spot lentigo is very common in the treatment of skin diseases. Surgery is the best method for treating lentigo with larger and darker spots.
Patients are to note down the changes in the appearance of pigmented nevi over a long period of time. If the pigmented nevus suddenly becomes bigger in size, gets dark in colour or has an irregular shape within a short period of time, and is also accompanied by pain, itching, and other uncomfortable symptoms, the patient should go to the doctor immediately to rule out the possibility of malignant melanoma.

The Role of Dermoscopy in Early Detection
Sun protection is a major measure in the prevention of skin problems, among which are the formation of ink spots, freckles and ink spot lentigo, while regular skin self-examination is a significant tool for skin problems. Through dermoscopy, doctors can more easily detect tiny lesions that are difficult to detect with the naked eye, and treat them in their early stages to avoid deterioration.
Early Signs of Ink Spot Lentigo
Ink Spot Lentigo presents early as a black or dark brown spot with an irregular shape. If the spot changes consistently in colour, size or shape, this should raise a red flag. Regular dermoscopic examinations enable dynamic monitoring of Ink Spot Lentigo and help doctors assess trends. If signs of malignancy or increased risk of malignancy are detected in Ink Spot Lentigo, doctors can take timely intervention to prevent the condition from worsening.
Application of New Techniques in Dermoscopy
Ink Spot Nevus appears dermoscopically as a dark brown to black irregular ink spot-like plaque. Through dermoscopy, doctors can assess the risk of malignant changes in nevus with ink spots, so as to formulate a more reasonable treatment plan.
As technology continues to advance, in the future, we can combine AI technology with dermoscopy to automate diagnosis and risk assessment by using algorithms to analyse colour, morphology and other features in dermoscopic images.