Article
Dermoscopy of Early Stage Melanoma
Melanoma develops from melanocytes, which are located in the epidermis of the skin. Melanoma can be display as changes of existing mole or a new spot on the skin. If not identified and treated early, melanoma is more likely to spread to other parts of the body. Melanoma can become life-threatening even in 6 weeks…
Early Stage Melanoma Detection Features via Dermoscopy - IBOOLO
IBOOLO's comprehensive guide on the dermoscopic features of early-stage melanoma provides expert strategies for timely diagnosis and treatment.
Dermoscopic Features of Early Stage Melanoma: A Comprehensive Clinical Guide
Early detection of melanoma through dermoscopy has revolutionized dermatological diagnosis, significantly improving survival rates through timely intervention. This comprehensive guide explores the crucial dermoscopic features that characterize early-stage melanoma, providing healthcare professionals with detailed insights for accurate diagnosis and treatment planning.
Understanding Early Stage Melanoma
Early-stage melanoma encompasses both in situ (Stage 0) and early invasive (Stage 1) melanoma. At these stages, the tumour is confined to the epidermis or has minimal dermal invasion, making it crucial for dermatologists to recognize subtle dermoscopic changes that may indicate malignant transformation.
Clinical Significance of Early Detection
- 5-year survival rate exceeds 95% when detected early
- Surgical margins can be minimized
- Reduced risk of metastatic spread
- Better cosmetic outcomes
- Lower treatment costs
Advanced Dermoscopic Features of Early Melanoma
1. Pigment Network Characteristics
The pigment network is one of the most significant dermoscopic features in early melanoma diagnosis.
Typical Features: Atypical Network Pattern, Irregularly distributed lines, Varying thickness of network lines, Abrupt network termination at the periphery, Dark brown to black colouration.
Key Variations: Negative network patterns, Pseudonetwork in facial lesions, Broadened network lines, Focal network disruption.
2. Vascular Patterns
Early melanoma often displays characteristic vascular features visible through dermoscopy.
Primary Vascular Indicators: Dotted Vessels, Irregular distribution, Varying vessel caliber, High density in certain areas. Linear Irregular Vessels, Serpentine pattern, Atypical arrangement, Color variation from pink to red.
3. Structural Components
Critical Structural Features: Dots and Globules, Irregular distribution, Varying sizes, Multiple Colors, Peripheral location. Streaks and Pseudopods, Irregular radial projections, Asymmetric distribution, Brown to black colouration. Blue-White Structures, Early regression signs, Scattered distribution, Mixed with pink areas.
Dermoscopic Algorithms for Early Melanoma
1. Pattern Analysis Method
This systematic approach evaluates Global Features, Reticular patterns, Globular patterns, Homogeneous patterns, Starburst patterns and Multicomponent patterns. Local Features, Network characteristics, Vascular structures, Specific local signs.
2. ABCD Rule of Dermoscopy
Enhanced scoring system for early detection: Asymmetry (A), Evaluation in two axes, Score 0-2 points. Border (B), Sharp cutoff assessment, Eight segments evaluation. Colour (C), Six potential colours, Scoring for each colour present. Differential Structures (D), Network patterns, Structureless areas, Dots, globules, streaks.
Special Considerations in Different Anatomical Locations
1. Facial Melanoma: Pseudonetwork pattern, Follicular openings, Asymmetric pigmentation, Annular-granular pattern.
2. Acral Melanoma: Parallel ridge pattern, Irregular diffuse pigmentation, Asymmetric structures, Multi-component pattern.
3. Amelanotic Melanoma: Atypical vessels, Pink to red colouration, Irregular dots and globules, Subtle structural changes.
Digital Dermoscopy and Follow-up
Sequential Digital Dermoscopy Imaging (SDDI)
1. Short-term monitoring: 3-month intervals, Documentation of changes, Early detection of evolution.
2. Long-term monitoring: 6-12 month intervals, Baseline comparison, Pattern evolution assessment.
3. Digital Documentation Standards: Standardized imaging conditions, Multiple image capture angles, Proper calibration and Color accuracy maintenance.
Advanced Diagnostic Technologies
1. Artificial Intelligence Integration: Pattern recognition algorithms, Deep learning applications, Automated risk assessment, Support for clinical decision-making.
2. Confocal Microscopy Correlation: Cellular-level imaging, Architecture assessment, Melanocyte visualization, Non-invasive staging.
Clinical Management Implications
Risk Stratification:
1. Low-risk features, Regular patterns, Symmetric structures, Single colour, Stable appearance.
2. High-risk features, Multiple patterns, Asymmetric structures, Multiple colours, Evolving appearance.
Treatment Planning: Surgical margin determination, Biopsy site selection, Follow-up scheduling, Management strategy development.
Future Directions
Emerging Technologies
1. 3D Dermoscopy: Volume assessment, Depth visualization, Enhanced structural analysis
2. Mobile Dermoscopy: Telemedicine applications, Remote monitoring, Patient self-monitoring.
Research Priorities: Biomarker correlation, Pattern recognition advancement, Artificial intelligence development, Outcome prediction models.
Dermoscopic examination of early-stage melanoma requires detailed knowledge of specific features and patterns. This comprehensive understanding, combined with systematic documentation and follow-up, enables early detection and improved patient outcomes. Continuous advancement in technology and diagnostic criteria further enhances our ability to identify and treat early melanoma effectively.
Recommended reading
How do I return or exchange my order – IBOOLO
Hassle-free Returns If for any reason you are unsatisfied, we gladly accept returns on most gear that is in its original undamaged packaging and products must be in new, mint condition within 15-days for a full refund of the purchased price. Returned or exchanged products must be in brand new, mint condition, and have all original...
Trusted OEM dermatoscope supplier making quality affordable - IBOOLO
IBOOLO an original dermatoscope equipment manufacturer (OEM), supplies high-quality skin screening tools at reasonable prices to distributors worldwide.
Download Letter of Designation – IBOOLO
Shenzhen Iboolo Optics Co.Ltd established in 2012, with more than 11+ years. We have been specialized in the field of Woods Lamp, Macro lens, Microscope and Dermatoscope, and so on. We are a high-tech company integrated with research, manufacture and marketing.
Melanoma develops from melanocytes, which are located in the epidermis of the skin. Melanoma can be display as changes of existing mole or a new spot on the skin. If not identified and treated early, melanoma is more likely to spread to other parts of the body. Melanoma can become life-threatening even in 6 weeks due to its aggressive speed of growth.
Hence, there is very crucial to inspect melanoma in its early stage. Dermoscopy is a very reliable and valuable aiding tool to identify and diagnose early melanoma. Dermoscopy enhances the confidence of dermatologists and patients, and also reduces the unnecessary biopsy and surgery.
What is melanoma?
Melanoma is a type of potential dangerous skin cancer that originates from melanocytes. Melanocytes are cells that are responsible for producing pigment melanin and give color to the skin. When melanocytes start to grow out of control, then melanoma arises. As a potential invasive skin cancer, melanoma can spread very quickly to other tissues of the body if left untreated.

What is early melanoma?
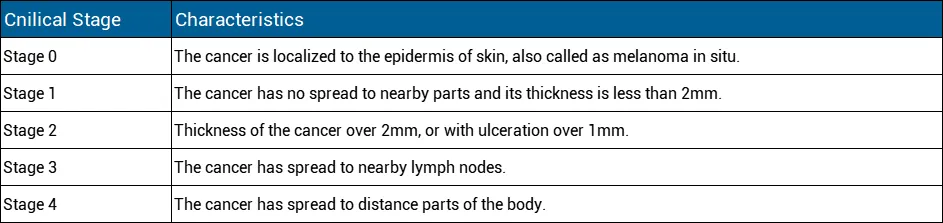
Early melanoma means it is on the early stage, has not spread. Stage of 0 and 1 are the early stage of melanoma
Stage 0: Stage 0 is the most noninvasive stage of melanoma, also called melanoma in situ. Such melanoma is located in the outermost layer of the skin and has not developed deeper.
Stage 1: Early melanoma, although also localized, becomes aggressive when it has penetrated the surface layer into the next layer of skin. At this point, the invasive tumor is less than 1 mm in size and may or may not ulcerate. When it is not ulcerated and is less than 0.8 mm in size, it is considered early and thin, also known as stage 1.
Epidemiology of melanoma
In the world, incidence rates of melanoma has been rising, especially like Australia and New Zealand reported as the highest rate of c
ountries. Western European and North America are following. Meanwhile, Asia and Africa have lower incidence rate of melanoma. As reported, melanoma is the third most common cancer in Australia and New Zealand. Melanoma is the fifth most common cancer in America.
Fair-skinned populations are the higher risk of groups than dark-skinned people in general.
High risk of melanoma
The main high risk factor for developing melanoma is over UV exposure, otherwise, there are some other high risk factors for producing melanoma as below:
Over UV exposure/history of sunburn
Fair-Skinned /white-skinned population
Family history
Existing moles
Increasing age
Weakened immune system
Clinical signs of early melanoma
The first clinical signs and symptoms of melanoma commonly are:
A change in an existing mole or freckle
The appearance of a new spot or atypical looking growth on the skin
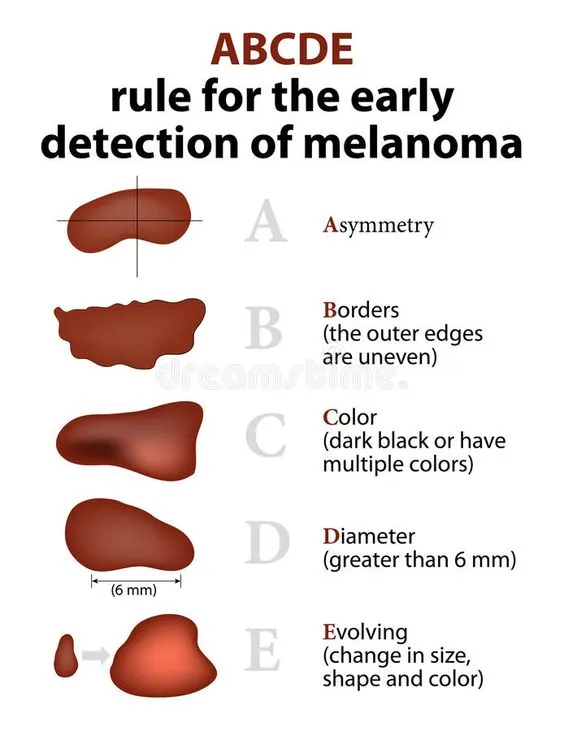
For early melanoma, there are famous “ABCDE” rules of the signs include: A: A is for Asymmetry. Melanoma often has irregular shapes and its two half are asymmetric. It means one half can not match the other. B: B is for Border. Border are irregular, blurred or ragged.
C: C is for Color. Colour is fulled with variation, or unusual colors, mixed colors and may change over the time.
D: D is for Diameter. Diameter of the spot is larger than 1/4inch (about 6millimeters)
E: E is for Evolving. Melanoma is change in its size, shape or color over time.
Stages of early melanoma
Stages of early melanoma can be complex, in summary, the stages are:
Dermoscopy of early stage melanoma
In clinical, some melanomas are extremely complex and difficult to identify. Especially in early stage of melanoma, its appearance in small size hard to detected. Dermoscopy plays a very important role to identify and diagnose the melanoma by combining a powerful lighting system and great magnification.
There are some certain features of early melanoma under dermoscopy including:
Asymmetrically distributed
Unusual pigment network
Irregular brown-black or multiple dots/globules
Blue-white veil
atypical vascular pattern or radial streaming
Scar-like depigmentation

What is the technique of dermoscopy?
Dermoscopy, also known as dermatoscopy or epiluminescence microscopy, is a dependable and useful medical device of helping skin doctors to diagnose various of skin lesions or skin diseases. Here’s the technique of dermoscopy as below:
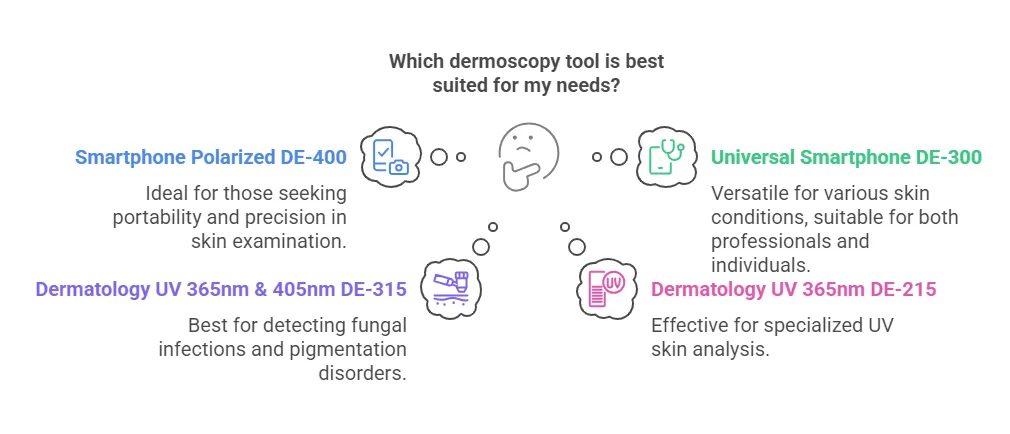
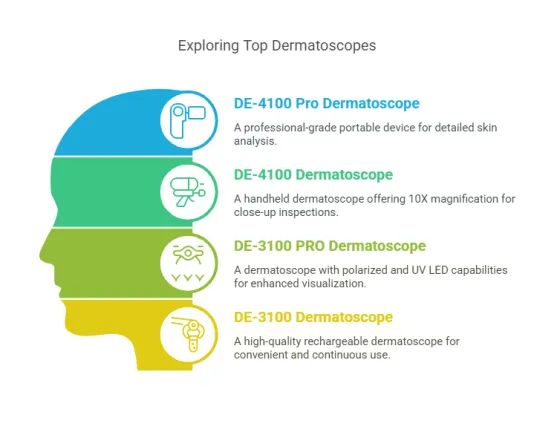
Instrument: Dermoscopy is commonly display as a handheld tool. This tool combines magnifying lens with a powerful lighting system to allow enhanced visualization with more details that are invisible by naked eyes. In addition, some dermoscopes is designed attached on a camera or a phone to directly observe or capture images of skin lesions.
Skin Preparation: Before the examination of dermoscopy, the patient’s skin should be keep clean. In some cases, if necessary, hair should be removed.
Application of Gel or Fluid: A gel or liquid (often alcohol or oil) may be applied to the skin lesion to reduce surface reflections and allows better visualization of deeper skin. But with the innovation and development of dermoscopy, there might no need any gel or liquid during the process of dermoscopy examination.

Observation of Structures: Dermoscopy reveals details of specific structures of the lesion to supply more valuable and key information for diagnosis.Such details include pigment networks, dots, globules, vessels, and other patterns.
Digital Imaging: Some dermoscopes are connected with a computer or a phone to capture digital images of the skin lesion. These images can be stored for later analysis and comparison.
Training and Expertise: It requires specialized and trained medical workers to interpret dermoscopic findings. Various patterns of dermatoscopic features of the lesion should be correlated with clinical context to get accurate and precise diagnosis.
How accurate is dermoscopy for melanoma?
Inspection by dermoscopy is more accurate than visual inspection alone in the diagnosis of melanoma.The accuracy of dermoscopy has been reported to range from 60% to 100%. But generally, Dermoscopy improved the accuracy of clinical diagnosis up to 35%.
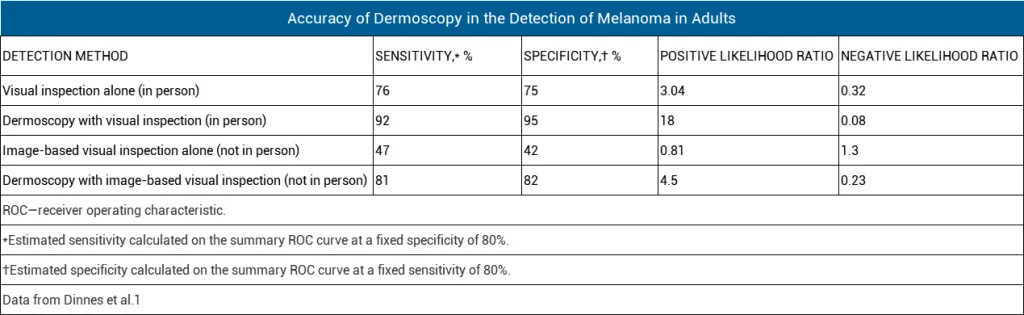
A 2018 Cochrane meta-analysis evaluated the diagnostic accuracy of dermoscopy in melanoma.
Advantages and disadvantages of dermoscopy for melanoma
As we can see, dermoscopy indeed can increase the sensitivity of diagnosis for melanoma.There are some advantages and disadvantages of for comparison dermoscopy with clinical examination(visual inspection):
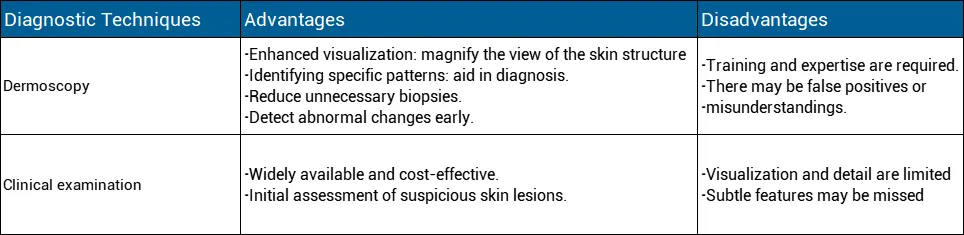
Compared with clinical examination, dermoscopy allows a brightening detail structures of skin lesion which are invisible by naked eyes. It is no doubt that dermoscopy can greatly increase the accuracy of diagnosis. In addition, dermatologist can store the images captured by dermoscope connected with phone or computer for later analysis and comparison. Dermoscopy plays a very significant role in the detection and diagnosis of skin lesion. People also need to learn how to use a dermoscopy to do self-examination in daily life . Any suspicious findings, have the skin checked by the professionals as soon as possible.