Article
Dermoscopy of Dermal Nevi
Dermal nevi may be present at birth or develop throughout life. These lesions are very common and can present in any individual. Dermal nevi appear in approximately 1% of newborns. Dermoscopy plays an important role as a common observation tool in dermatology that helps doctors observe the deep structure of dermal pigmented nevi. Overview of…
Dermal nevi may be present at birth or develop throughout life. These lesions are very common and can present in any individual. Dermal nevi appear in approximately 1% of newborns. Dermoscopy plays an important role as a common observation tool in dermatology that helps doctors observe the deep structure of dermal pigmented nevi.
Overview of Dermal Nevi
A dermal nevus is a benign, well-defined, raised, colored, papule that appears on the surface of the skin. Dermal nevi can be brown, tan, black, reddish-brown, purple, or skin-colored, and are generally round or ovoid . They may be sessile, raised, and have hair growing from them.
Moreover, dermal nevi are usually benign skin lesions formed by melanocytes in the skin that accumulate in the dermis. Most dermal nevi are stable and do not undergo malignant changes. So, most people don’t need to be alarmed if they find a dermal pigmented nevus on their body.

Principles of Dermoscopy Examination
A dermatoscope is a handheld device, equipped with a magnification lens and a light source. It enables the visualization of the subsurface morphology of cutaneous lesions, down to the depth of the superficial dermis. It reveals colors and structures that are normally not visible to the unaided eye and improves the diagnostic accuracy.
Preparation before Digital Dermoscopy Examination
Before the start of dermoscopy, the patient needs to clean the skin surface to be examined in advance, and inform the doctor if there is any local inflammation or breakage, so that the doctor can assess the suitability of dermoscopy. During the examination, the doctor will put the probe of the dermatoscope on the surface of the skin lesion that needs to be observed, keeping a good distance between the probe and the skin. Adjust the light source and magnification of the device until the picture is clear. The doctor will select representative areas of dermal nevus for examination, including the edges and centre of the lesion as well as the surrounding normal skin areas for comparative analysis.
Steps in Dermoscopy
When performing a dermoscopy, first the doctor will select a typical area of dermal nevus skin. Next, gently place the probe of the dermatoscope on the skin surface to be observed, rotate and adjust the focus until the image is clear. Observe the structure and colour changes of the lesions through dermoscopy, and determine the type and degree of progression of the lesions based on the observations. If you want to save the image, you can point the mobile phone clip to the main camera of the mobile phone, then connect the magnetic ring option to the mobile phone clip, and finally connect the dermatoscope magnetically. Switch on the camera function of the mobile phone to save the image. Failure to acquire a dermatoscope image may result if you make a mistake during the operation.

Digital Dermoscopy of Dermal Nevi
The pigment cells of dermal pigmented nevi are mainly distributed in the dermis, usually located in the upper or middle part of the dermis. These pigment cells can be seen dermoscopically usually arranged in clusters, forming islands, curved or scattered within the dermis and even sometimes deep into the subcutaneous tissue. There are several different types of dermal pigmented nevi, including but not limited to:
Flat dermal pigmented nevi:
These nevi are usually smaller, more regular in shape, and commonly found in adult skin.
Nodular dermal nevus:
Nodular dermal naevi are usually larger and often form elevations on the surface of the skin, and can even be felt as hard nodules.
Mixed dermal pigmented nevus:
This type of nevus has mixed features of epidermis and dermis, and pigment cells can be observed under dermoscopy to exist between epidermis and dermis at the same time.
How to Analyse Colours, Patterns, Boundaries and Structures in Digital Dermoscopic Images
Colour:
In dermatology microscopy images, the density and distribution of pigmentation often determines the colour of its appearance. Typically, dermal nevi appear dark brown to black, or lighter if the pigment cells are more dispersed.
Pattern:
Observe the pattern of pigment cell arrangement in the image; normal dermal pigmented nevi appear as regular clusters and may have a more uniform distribution of structures.
Border:
Dermal pigmented nevi usually have clear borders and do not easily penetrate into the surrounding tissues. On the other hand, malignant melanoma, for example, may show irregular, fuzzy borders and may show signs of infiltration or expansion into other layers of the skin.
Structure:
Normal dermal pigmented nevus cells are relatively neatly arranged and the stroma appears normal, whereas abnormal hyperplasia or stromal changes may suggest pathological changes.

Diagnosis and Management of Dermal Nevi
Dermal nevi are benign. Even though benign nevi do not pose health risks such as melanomas, many people opt to have them removed. Most people who seek to have nevi removed do so for cosmetic reasons, for instance, if one is embarrassed about how a particular mole or moles look.
Common methods of removing nevi include: the nevus can be cut off the skin. Some nevi may have subcutaneous cells, which reside underneath the skin, so the doctor might need to make a deeper cut to remove the entire mole to prevent it from growing back. The cut may require stitches.
Differentiation of Dermal Nevi from Other Skin Lesions
Dermal nevi with this clinical morphology will usually reveal one or more of the following dermoscopic features: comma vessels, brown halo, globules, small foci of tan structureless pigmentation, hypopigmented areas. They can also reveal arborizing vessels making it difficult to differentiate them from BCC. The clues to the diagnosis of dermal nevi include the presence of the aforementioned features and lack of other BCC-specific features. In addition, the arborizing vessels in dermal nevi are often a tad out of focus and have a bluish hue. In contrast, in BCC the arborizing vessels are usually sharply in focus and bright red in color.

Application of New Techniques in Digital Dermoscopy
Artificial intelligence (AI) can be defined as the branch of computer science dealing with the simulation of intelligent human behavior in computers. Dermatology has taken the leading position for the implementation of AI in the medical field because of its large clinical, dermoscopical, and dermatopathological image database.
In 2017, Stanford university published a study on deep learning of skin tumors. They trained CNN, using more than 1 lakh images of around 2000 different diseases and tested its performance against that of 21 board-certified dermatologists on biopsy-proven clinical images. It was found that machine had a competence, comparable to that of board-certified dermatologists in identifying and classifying skin cancers.
Conclusion
Dermoscopy contributes to a better visualisation of the deeper components of the skin and assists in the accurate diagnosis of dermal Nevi, including its type, size and distribution, in order to establish more targeted treatment. Doctors can differentiate dermal nevi with other pigmented skin diseases using dermoscopic image analysis and can avoid misdiagnosis after that. Dermoscopy is a promising approach to improving the diagnostic accuracy and efficiency of dermal nevi and other skin diseases with continuous education and technological innovation as important drivers for the continuous development of dermoscopy.
Dermal Nevi Dermoscopy, Digital Dermoscopy: Skin Diagnosis Tools
Dermal nevi dermoscopy and digital dermoscopy enhance skin diagnosis with high-resolution imaging and AI. They detect melanoma, track nevi changes, and improve accuracy. Essential for modern dermatology practices.
Dermal Nevi Dermoscopy and Digital Dermoscopy: Revolutionizing Skin Lesion Diagnosis and Monitoring
Digital dermoscopy has transformed the way dermatologists diagnose and monitor dermal nevi, offering unparalleled precision and efficiency. By combining high-resolution imaging, advanced lighting, and AI-powered analysis, this technology enables early detection of melanoma and other skin conditions. From mapping multiple nevi to tracking subtle changes over time, digital dermoscopy provides a comprehensive solution for skin lesion management. This blog explores its clinical applications, essential features, and best practices for integration into dermatology practices. Whether you're new to digital dermoscopy or looking to optimize its use, this guide will help you harness its full potential for improved patient outcomes.
What is Digital Dermoscopy and How Does it Transform Dermal Nevi Examination?
Digital dermoscopy is an advanced imaging technique that combines traditional dermoscopy with digital technology to enhance the examination of dermal nevi (skin moles). Unlike conventional methods, digital dermoscopy allows for high-resolution imaging, storage, and analysis of skin lesions over time.
How Does it Transform Dermal Nevi Examination?
- High-Resolution Imaging: Captures detailed images of nevi, enabling precise analysis of structure and pigmentation.
- Longitudinal Tracking: Stores images for comparison over time, helping detect subtle changes that may indicate malignancy.
- AI Integration: Some systems use artificial intelligence to assist in diagnosing suspicious lesions, improving accuracy.
Why is Digital Dermoscopy a Game-Changer?
It provides dermatologists with a powerful tool for early detection of melanoma and other skin cancers, significantly improving patient outcomes.
The Complete Guide to Dermoscopy Technology for Monitoring and Analyzing Dermal Nevi
Dermoscopy technology has revolutionized the way dermatologists monitor and analyze dermal nevi, offering a non-invasive and highly accurate method for skin lesion evaluation.
What Makes Dermoscopy Technology Effective?
- Polarized Lighting: Reduces surface glare, allowing for a clearer view of subsurface structures.
- Magnification: Provides up to 10x magnification, revealing details invisible to the naked eye.
- Digital Integration: Enables image storage, analysis, and sharing for collaborative diagnosis.
How to Use Dermoscopy for Dermal Nevi Monitoring:
1. Capture Baseline Images: Take high-resolution images of all nevi during the initial examination.
2. Analyze Lesion Features: Use dermoscopic criteria (e.g., asymmetry, color, and structure) to assess nevi.
3. Schedule Follow-Ups: Regularly compare new images with baseline images to monitor changes.
Why is This Technology Essential?
It enhances diagnostic accuracy and provides a reliable method for tracking nevi over time, ensuring early detection of potential issues.
How Digital Dermoscopy Systems Work: The Technology Behind Enhanced Skin Lesion Visualization
Digital dermoscopy systems combine advanced optics, lighting, and software to provide unparalleled visualization of skin lesions.
What Are the Key Components of Digital Dermoscopy Systems?
- High-Resolution Camera: Captures detailed images of skin lesions.
- Polarized Light Source: Illuminates the skin to reveal subsurface structures.
- Software Integration: Allows for image storage, analysis, and comparison over time.
How Does the Technology Work?
1. Image Capture: The camera takes a high-resolution image of the lesion under polarized light.
2. Image Analysis: Software enhances the image and highlights key features, such as pigment patterns and vascular structures.
3. Data Storage: Images are stored in a database for future reference and comparison.
Why is This Technology Revolutionary?
It provides dermatologists with a powerful tool for accurate diagnosis and long-term monitoring of skin lesions.
Step-by-Step Tutorial: Conducting Thorough Dermal Nevi Assessment Using Digital Dermoscopy
A thorough dermal nevi assessment using digital dermoscopy involves several key steps to ensure accurate diagnosis and monitoring.
How to Perform a Dermal Nevi Assessment:
1. Prepare the Patient: Clean the skin area and ensure the patient is comfortable.
2. Capture Baseline Images: Use the digital dermoscopy system to take high-resolution images of all nevi.
3. Analyze Lesion Features: Examine the images for asymmetry, irregular borders, color variations, and structural abnormalities.
4. Document Findings: Record observations and store images in the patient’s file for future reference.
5. Schedule Follow-Ups: Plan regular follow-up appointments to monitor any changes in the nevi.
Why is This Process Important?
Following these steps ensures a comprehensive evaluation of dermal nevi, enabling early detection of potential issues.
Digital vs. Traditional Dermoscopy: Comparing Accuracy in Melanocytic Nevi Diagnosis
Digital and traditional dermoscopy are both valuable tools for diagnosing melanocytic nevi, but they differ significantly in terms of accuracy and functionality.
What Are the Key Differences?
- Image Quality: Digital dermoscopy provides higher-resolution images compared to traditional methods.
- Data Storage: Digital systems allow for image storage and comparison over time, while traditional dermoscopy relies on visual memory.
- AI Assistance: Some digital systems incorporate AI to assist in diagnosis, improving accuracy.
How Do They Compare in Accuracy?
- Digital Dermoscopy: Offers superior accuracy due to high-resolution imaging and the ability to track changes over time.
- Traditional Dermoscopy: Relies on the dermatologist’s expertise and may miss subtle changes without digital aids.
Why Choose Digital Dermoscopy?
Digital dermoscopy provides a more accurate and reliable method for diagnosing and monitoring melanocytic nevi, making it the preferred choice for modern dermatology practices.
The Clinical Applications of Digital Dermoscopy Beyond Melanoma Detection
Digital dermoscopy is widely known for its role in melanoma detection, but its applications extend far beyond this critical function.
What Are the Other Clinical Uses of Digital Dermoscopy?
- Non-Melanoma Skin Cancers: Detects basal cell carcinoma and squamous cell carcinoma by analyzing vascular patterns and lesion structures.
- Inflammatory Skin Conditions: Helps differentiate between psoriasis, eczema, and other inflammatory diseases based on dermoscopic features.
- Infectious Skin Diseases: Identifies fungal infections, scabies, and viral warts through characteristic patterns.
- Hair and Scalp Disorders: Assists in diagnosing conditions like alopecia and folliculitis by examining scalp lesions and hair follicles.
Why is Digital Dermoscopy Versatile?
Its ability to provide detailed, high-resolution images makes it a valuable tool for diagnosing a wide range of skin conditions, improving accuracy and patient outcomes.
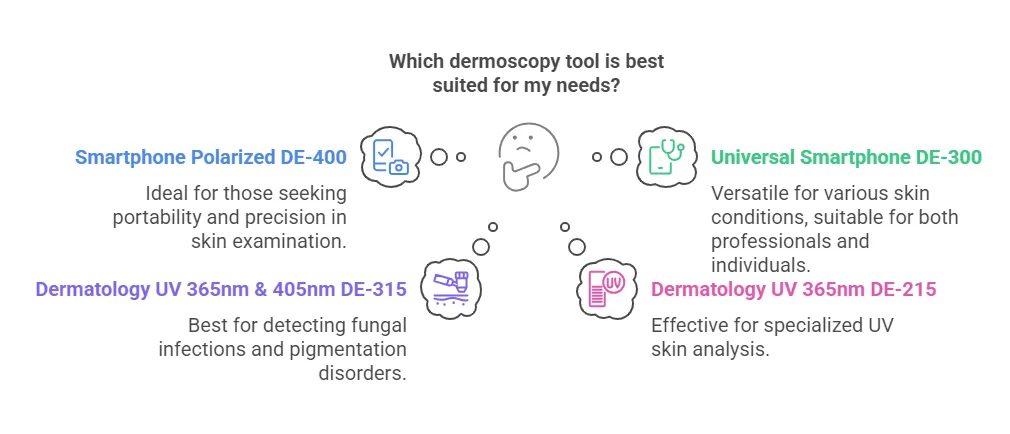
Essential Features to Look for When Investing in a Digital Dermoscopy System
Choosing the right digital dermoscopy system is crucial for enhancing diagnostic accuracy and workflow efficiency.
What Features Should You Prioritize?
- High-Resolution Imaging: Look for systems with at least 10x magnification and high-definition cameras for clear, detailed images.
- Polarized Lighting: Ensures better visualization of subsurface structures by reducing surface glare.
- User-Friendly Software: Opt for systems with intuitive software for image storage, analysis, and comparison over time.
- Portability: Consider lightweight, handheld devices for ease of use in clinical settings.
- AI Integration: Advanced systems with AI capabilities can assist in lesion analysis, improving diagnostic accuracy.
Why Are These Features Important?
Investing in a system with these features ensures reliable performance, enhances diagnostic capabilities, and streamlines patient care.
Maintenance and Care Guidelines for Preserving Digital Dermoscopy Equipment Longevity
Proper maintenance is essential to ensure the longevity and optimal performance of digital dermoscopy equipment.
How to Maintain Your Digital Dermoscopy System:
1. Regular Cleaning:
- Wipe the camera lens and body with a soft, lint-free cloth.
- Use a lens cleaning solution to remove smudges or fingerprints.
2. Check for Damage:
- Inspect cables, connectors, and the device body for wear and tear.
- Replace damaged components promptly.
3. Update Software:
- Ensure the system’s software is up-to-date to benefit from the latest features and security patches.
4. Store Properly:
- Keep the device in a protective case when not in use to prevent dust accumulation and physical damage.
5. Calibrate Regularly:
- Follow the manufacturer’s guidelines for calibration to maintain image accuracy.
Why is Maintenance Critical?
Regular care prevents malfunctions, extends the equipment’s lifespan, and ensures consistent diagnostic accuracy.
Understanding Dermoscopic Patterns: A Comprehensive Guide to Dermal Nevi Classification
Dermoscopic patterns play a crucial role in classifying dermal nevi and differentiating them from malignant lesions.
What Are the Key Dermoscopic Patterns?
- Reticular Pattern: Characterized by a network of lines, commonly seen in benign nevi.
- Globular Pattern: Features round or oval structures, often found in congenital nevi.
- Homogeneous Pattern: Shows uniform coloration, typical of intradermal nevi.
- Starburst Pattern: Exhibits radial streaks, often associated with Spitz nevi.
- Atypical Pattern: Displays irregular structures, colors, or borders, which may indicate malignancy.
How to Classify Dermal Nevi Using Dermoscopy:
1. Capture High-Quality Images: Use a digital dermoscopy system to obtain clear images of the lesion.
2. Analyze Patterns: Compare the lesion’s features with known dermoscopic patterns.
3. Document Findings: Record observations and classify the nevus based on its pattern.
Why is Pattern Recognition Important?
Understanding these patterns helps dermatologists accurately classify nevi, reducing the risk of misdiagnosis and unnecessary biopsies.
How Artificial Intelligence is Enhancing Digital Dermoscopy Accuracy and Efficiency
Artificial intelligence (AI) is revolutionizing digital dermoscopy by improving diagnostic accuracy and streamlining workflows.
What Role Does AI Play in Digital Dermoscopy?
- Automated Lesion Analysis: AI algorithms analyze dermoscopic images to identify patterns indicative of malignancy.
- Risk Stratification: AI can classify lesions into low, medium, or high-risk categories, aiding in decision-making.
- Image Enhancement: AI improves image quality by reducing noise and enhancing details.
- Data Integration: AI systems can integrate patient history and dermoscopic findings for a comprehensive diagnosis.
How Does AI Improve Accuracy and Efficiency?
- Reduces Human Error: AI minimizes subjective interpretation, leading to more consistent diagnoses.
- Saves Time: Automates repetitive tasks, allowing dermatologists to focus on complex cases.
- Enhances Early Detection: Improves the identification of early-stage malignancies, increasing treatment success rates.
Why is AI a Game-Changer?
By combining AI with digital dermoscopy, dermatologists can achieve higher diagnostic accuracy, improve patient outcomes, and optimize clinical workflows.
Digital Dermoscopy Integration into Dermatology Practice: Workflow Optimization Strategies
Integrating digital dermoscopy into a dermatology practice can significantly enhance diagnostic accuracy and streamline workflows.
How to Optimize Workflow with Digital Dermoscopy:
1. Train Staff: Ensure all team members are proficient in using the digital dermoscopy system.
2. Standardize Protocols: Develop consistent procedures for image capture, analysis, and storage.
3. Integrate with EMR: Connect the dermoscopy system to your electronic medical records (EMR) for seamless data management.
4. Schedule Regular Reviews: Set aside time for reviewing and comparing dermoscopic images to monitor changes in lesions.
5. Leverage AI Tools: Use AI-powered features for automated lesion analysis and risk assessment.
Why is Workflow Optimization Important?
Efficient integration of digital dermoscopy improves diagnostic accuracy, reduces administrative burden, and enhances patient care.
Mapping and Monitoring Multiple Dermal Nevi: Digital Dermoscopy Best Practices
Monitoring multiple dermal nevi is a common challenge in dermatology, but digital dermoscopy offers effective solutions.
What Are the Best Practices for Mapping and Monitoring Nevi?
1. Create a Baseline: Capture high-resolution images of all nevi during the initial examination.
2. Use Body Maps: Document the location of each nevus on a body map for easy reference.
3. Schedule Follow-Ups: Regularly compare new images with baseline images to detect changes.
4. Prioritize High-Risk Nevi: Focus on nevi with atypical features or those in high-risk patients.
5. Utilize Software Features: Take advantage of digital tools for image annotation, measurement, and side-by-side comparisons.
Why is Systematic Monitoring Crucial?
It ensures early detection of malignant changes, reduces the risk of missed diagnoses, and provides a clear record for patient management.
Quality Considerations and Usage Precautions for Digital Dermoscopy in Clinical Settings
To maximize the benefits of digital dermoscopy, it’s essential to adhere to quality standards and usage precautions.
What Are the Key Quality Considerations?
- Image Resolution: Ensure the system provides high-resolution images for accurate analysis.
- Lighting Consistency: Use polarized lighting to minimize glare and enhance subsurface details.
- Calibration: Regularly calibrate the device to maintain image accuracy.
What Usage Precautions Should Be Taken?
- Patient Comfort: Ensure the patient is comfortable and the skin is clean before imaging.
- Device Handling: Avoid dropping or mishandling the device to prevent damage.
- Data Security: Protect patient data by using secure storage and transfer methods.
Why Are These Considerations Important?
Adhering to quality standards and precautions ensures reliable results, protects patient data, and extends the lifespan of the equipment.
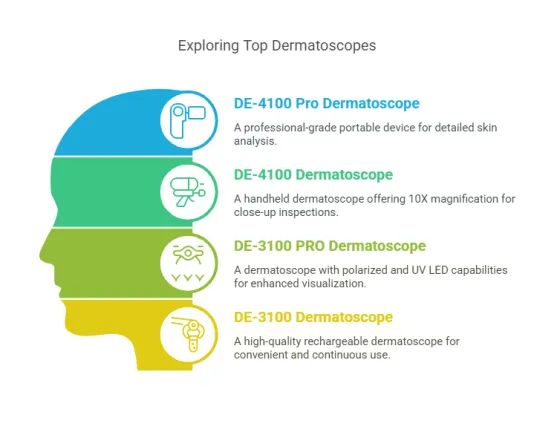
The Evolution of Dermoscopy: From Handheld Devices to Advanced Digital Imaging Systems
Dermoscopy has evolved significantly, transitioning from simple handheld devices to sophisticated digital imaging systems.
How Has Dermoscopy Evolved?
- Early Handheld Devices: Basic magnifying tools with limited lighting options.
- Polarized Dermoscopy: Introduced polarized lighting to reduce glare and improve visibility.
- Digital Dermoscopy: Combined high-resolution imaging with software for analysis and storage.
- AI Integration: Added artificial intelligence for automated lesion analysis and risk assessment.
Why is This Evolution Significant?
Advanced digital dermoscopy systems provide unparalleled diagnostic accuracy, making them indispensable in modern dermatology.
Comparative Analysis of Digital Dermoscopy Platforms for Comprehensive Nevi Documentation
Choosing the right digital dermoscopy platform is crucial for effective nevi documentation and analysis.
What Factors Should Be Compared?
- Image Quality: High-resolution imaging is essential for detailed analysis.
- Software Features: Look for platforms with annotation, measurement, and comparison tools.
- Ease of Use: User-friendly interfaces streamline workflows and reduce training time.
- AI Capabilities: Platforms with AI integration offer enhanced diagnostic accuracy.
- Cost and Support: Consider the total cost of ownership and the availability of technical support.
How to Choose the Best Platform:
1. Define Your Needs: Identify the specific features and capabilities required for your practice.
2. Compare Options: Evaluate multiple platforms based on image quality, software features, and cost.
3. Test Before Buying: Request a demo or trial period to assess the platform’s performance.
Why is a Comparative Analysis Important?
It ensures you select a platform that meets your practice’s needs, enhancing diagnostic accuracy and workflow efficiency.
This blog delves into the transformative role of digital dermoscopy in diagnosing and monitoring dermal nevi. It highlights how high-resolution imaging, polarized lighting, and AI integration enhance diagnostic accuracy and streamline workflows. Key topics include the evolution of dermoscopy technology, best practices for mapping and monitoring nevi, and essential features to consider when investing in a digital dermoscopy system. Additionally, the article covers maintenance guidelines, clinical applications beyond melanoma detection, and the impact of AI on diagnostic efficiency. By understanding and leveraging these advancements, dermatologists can improve early detection rates, optimize patient care, and stay at the forefront of skin lesion management.