Article
Dermoscopy of Clear Cell Acanthoma
Clear cell acanthoma is a very rare benign epithelial tumor that is mainly caused by excessive glycogen accumulation in the epidermal keratinocytes. The lesions are characterized by a limited brown or red moist soft nodules having well defined edges and a smooth, dry flaky surface. And they develop without such symptoms as feeling pain or…
Clear cell acanthoma is a very rare benign epithelial tumor that is mainly caused by excessive glycogen accumulation in the epidermal keratinocytes. The lesions are characterized by a limited brown or red moist soft nodules having well defined edges and a smooth, dry flaky surface. And they develop without such symptoms as feeling pain or itching.
What Is Clear Cell Acanthoma?
Clear cell acanthoma also called as pale cell echinoderma or Degos echinoderma, is a tumefying one with elevation of single or multiple red-brown firm papules measuring about 0.5–2 cm in diameter. Usually, patients who have such skin diseases do not feel itchy; thus, they seldom perceive the disease presence. Clear cell acanthoma is a benign tumor that does not become malignant.
The exact pathogenesis of clear cell acanthoma has not been completely established despite knowledge that it involves a type of tumor made up of abnormal glycogen accumulation in the epidermal keratinocytes. Histologically, it has been shown to have features like hypertrophy of the epidermal stratum spinosum along with pale transparent larger polygonal keratinocytes, which are separated from normal adjacent epidermal cells by well-defined boundaries. It appears that middle-aged individuals over 40 years old are more prone to this condition compared to young adults, while males are more likely to be affected than females.
What Is the Etiology of Clear Cell Acanthoma?
Though the medical community has yet to reach a consensus regarding the root causes of clear cell acanthoma, which is treated as a rare skin disease, the disease is widely accepted as such. As a rule, it is usually believed to be a condition resulting from a surplus of glycogen that builds up in keratinocytes of the epidermis. But, the reason for the excess of glycogen in the dermal keratinocytes of clear cell acanthoma is still unclear. A genetic relationship might be the cause of the disease.

The Role of Dermoscopy in the Diagnosis of Clear Cell Acanthoma
Dermatoscope is a tool that combines magnification and polarised light to magnify a certain number of times and filter the refracted light from the skin’s surface stratum corneum. Doctors can use it to observe very clear structures and details of the skin.
First, clean the skin of the area you will be seeing with a cleanser to remove oil, dirt, and the residue before using your dermatoscope. Dermatoscope set magnification and distance of the focus according to necessity. Place it in the area where you just cleaned your skin and at a good distance and angle. Inspect the surface skin from various angles of the skin pattern.
Clear cell acanthoma may be misdiagnosed as seborrheic keratosis and some other skin conditions. However, dermoscopy can reveal some of the features of clear cell echinoderma, i.e., blood vessels arranged in a pearly or creeping pattern that look like glomerular or punctate and glomerulonodular blood vessels, which can help doctors to make a correct differential diagnosis.
Typical Dermoscopic Features of Clear Cell Acanthoma
Vascular pattern:Tiny, round, uniform dotted vessels and a continuous tandem network-like arrangement in the superficial plane of the lesion forming the “string-of-pearls” pattern.
Lesion morphology: The lesion is usually a well-delimited, slightly elevated papule or nodule.
Color variation: Usually skin colored to light red or light brown. At dermoscopy, the color distribution within the lesion may sometimes be uneven, but an obvious pigmentary change is in general not observed.

Dermoscopic Differences between Early and Mature Clear Cell Acanthoma
Clear cell acanthoma often has the anterior or creeping distribution of glomeruloid blood vessels, presenting as an appearance like “beads” on a dermoscopic image — this is one prime example . In the process of advancement, a clear cell acanthoma of an advanced phase may develop a non-homogeneous white crosshatched line, with the lines being of different widths. These lines of the lesion may be related to fibroblast tissue proliferation or keratinization. The full form clear cell acanthoma may demonstrate the presence of thick contour coiled blood vessels associated with red clots which were attributed to vasodilatation and congestion occurring within the lesion.
Clear Cell Acanthoma and Other Skin Lesions
Clear Cell Acanthoma (CCA)
Clinical Features: Usually presents itself in a solitary, well-circumscribed, red to brown nodules or plaques mostly on the lower legs.
Dermoscopy: String of Pearls Pattern, Pale Pink Background, Shiny White Lines and Glomerular Vessels
Basal Cell Carcinoma (BCC)
Clinical Features: It usually shows itself as a pearly or translucent nodule with telangiectasia. It can ulcerate and easily bleed.
Dermoscopy: Arborizing Vessels, Blue-Gray Ovoid Nests, Leaf-Like Areas and Ulceration
Squamous Cell Carcinoma (SCC)
Clinical Features: A scaly, red patch, nodule, or plaque that may ulcerate is presented. Found mostly on sun-exposed areas.
Dermoscopy: Keratin Masses, Glomerular Vessels and White Circles
Key Differentiating Points
Vascular Patterns: The CCA has a “string of pearls” pattern which is astonishingly different from the other two tumors; BCC with its many thin branching arteries and SCC whose glomerular vessel looks like a spider’s.
Background Color: CCA has a uniform pale pink background while BCC has a translucent or pearly sheen and SCC is mostly scaly with a red shade.
Surface Features: The peripheral collarette of scale in CCA is a distinctive characteristic and it is not usually present in BCC and SCC.

Treatment Options and Prognosis for Clear Cell Acanthoma
Given that clear cell acathom a is quite deep, it should be surgically excised. Non-surgical treatments are mostly laser therapy, cryotherapy, electrocoagulation and drugs. The prognosis of clear cell acanthoma is generally good, for it mad be a benign bemignant skin tumor with slow growth and low malignancy transformation to become canceraceous which has relatively lower recurrence after treatment. The sores cannot be scratched to avoid injury, and once again will perform as needed if it is found out that the changes are abnormal.
Prevention of Clear Cell Acanthoma and Regular Dermoscopic Screening
In order not to trigger the outbreak of clear cell acanthoma, we should equip our skin with proper hygiene and avoid too much exposure to the sun which is not friendly as ultraviolet radiation is among the causes of many skin lesions. Furthermore, the immune system can be strengthened through the regular diet and moderate exercise, which will serve as a shield against skin lesions.
Through dermatoscopic screenings, skin complications can be recognized at a very early stage, even in the case of clear cell acantholysis, which leads to significantly better results in treatment. By the way, the increased awareness of skin health through the timely detection of lesions is another benefit of regular dermoscopic screenings.
Clear Cell Acanthoma Dermoscopy: A Comprehensive Analysis from Diagnosis to Follow-up
Clear Cell Acanthoma (CCA) is a rare benign skin tumour that can clinically mimic malignant lesions, making accurate diagnosis crucial. Dermoscopy, as a non-invasive tool, magnifies the lesion area and reveals characteristic features such as a "cobblestone-like" surface and regular vascular patterns, providing essential support for CCA diagnosis. This article will explore in depth the application of dermoscopy in clear cell acanthoma, including its working principles, diagnostic advantages, latest research advances, and screening practices in primary care institutions, helping readers comprehensively understand the value of this technology in skin tumour management.
What is Clear Cell Acanthoma?
Clear Cell Acanthoma (CCA) is a rare benign skin tumor typically presenting as a solitary, red or brown papule or plaque. It most commonly occurs on the lower extremities of middle-aged and elderly individuals, particularly on the shin. Although CCA is benign, its clinical appearance may sometimes resemble malignant skin tumors, making accurate diagnosis essential. Dermoscopy, as a non-invasive diagnostic tool, helps physicians observe lesion details more clearly, facilitating diagnosis.
Why is Dermoscopy Important for Clear Cell Acanthoma?
Dermoscopy plays a crucial role in diagnosing clear cell acanthoma. Through dermoscopy, physicians can observe typical CCA features such as a "cobblestone-like" surface structure and regular vascular patterns. These characteristics help differentiate CCA from other skin lesions, reducing the possibility of misdiagnosis. Additionally, clear cell acanthoma dermoscopy does not require tissue biopsy, minimizing patient discomfort and is particularly suitable for patients concerned about biopsies.
How Does Dermoscopy Work for Clear Cell Acanthoma?
Dermoscopy works by magnifying the lesion area and using polarized light or liquid medium to reduce skin surface reflection, allowing physicians to observe structures in the epidermis and upper dermis more clearly. For clear cell acanthoma, typical dermoscopic features include:
Cobblestone-like surface: The lesion surface appears as uniform granular structures similar to cobblestones.
Regular dotted or comma-shaped vessels: Vessels are evenly distributed, regular in shape, usually appearing red or purple.
Well-defined borders: Clear boundaries between the lesion and surrounding normal skin, with regular edges.
These features help physicians make preliminary diagnoses without the need for biopsies.
Can Dermoscopy Improve the Diagnosis of Clear Cell Acanthoma?
Clear cell acanthoma dermoscopy significantly improves diagnostic accuracy. Traditional clinical diagnosis relies on naked-eye observation, which can easily confuse CCA with other skin lesions such as basal cell carcinoma or melanoma. Dermoscopy provides more detailed information about the lesion, helping physicians identify unique CCA features. Furthermore, dermoscopic examination can be used to monitor lesion changes, particularly during post-treatment follow-up, evaluating whether the lesion has completely resolved or recurred.
How to Perform Dermoscopy for Clear Cell Acanthoma: Step by Step
Performing clear cell acanthoma dermoscopy requires following these steps:
1. Preparation: Clean the lesion area, ensuring the skin surface is free of oils or dirt.
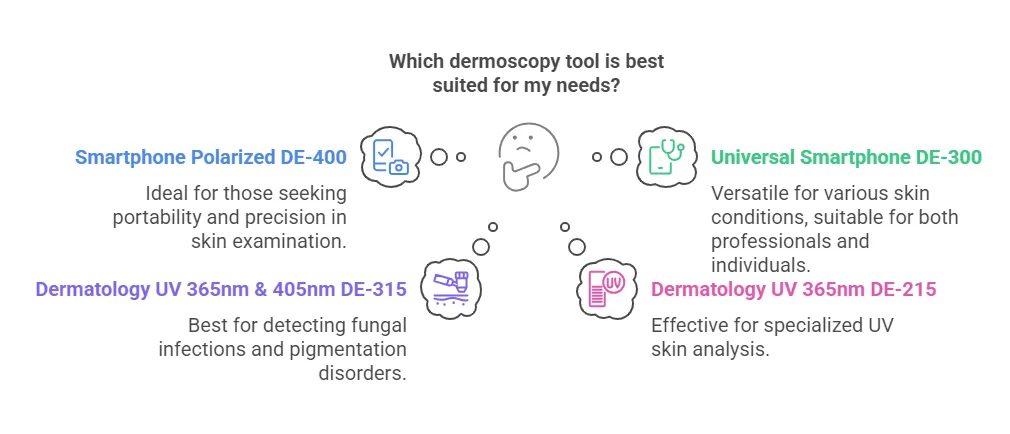
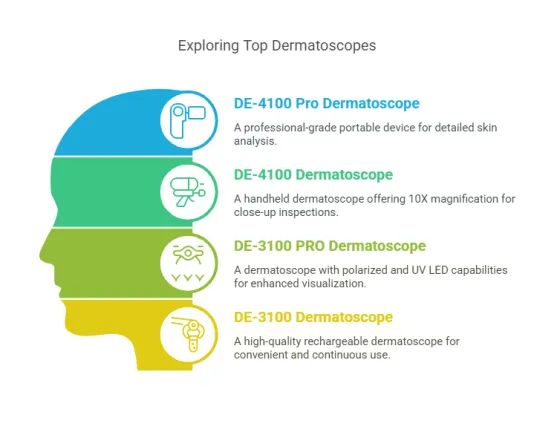
2. Select appropriate dermoscope: Choose a handheld or desktop dermoscope based on the location and size of the lesion.
3. Apply medium: Apply a coupling agent (such as alcohol or gel) to the lesion area to reduce skin surface reflection.
4. Observe the lesion: Carefully examine the lesion's surface structure, vascular patterns, and border characteristics using the dermoscope.
5. Record results: Take dermoscopic images and document observed features for subsequent analysis and diagnosis.
By following these steps, physicians can more accurately assess clear cell acanthoma characteristics and make correct diagnoses.
Does Dermoscopy Have Limitations in Diagnosing Clear Cell Acanthoma?
Although clear cell acanthoma dermoscopy offers significant advantages in diagnosis, it also has certain limitations. For instance, some atypical CCAs may lack typical dermoscopic features, making diagnosis difficult. Additionally, dermoscopic examination results depend on the physician's experience and skills; inexperienced physicians may misinterpret lesions. Therefore, histopathological examination should be combined when diagnosis is uncertain to confirm the diagnosis.
What Are the Clinical Applications of Dermoscopy for Clear Cell Acanthoma?
Clear cell acanthoma dermoscopy has wide clinical applications, including:
Preliminary diagnosis: Helping physicians make initial judgments about whether a lesion is CCA by observing dermoscopic features.
Differential diagnosis: Distinguishing CCA from other similar skin lesions, such as seborrheic keratosis or basal cell carcinoma.
Treatment monitoring: Using dermoscopy after treatment to monitor lesion changes and evaluate treatment effectiveness.
Patient education: Explaining the nature of the lesion and treatment plans to patients by showing dermoscopic images, enhancing patient understanding and cooperation.
These applications make dermoscopic examination an important tool in the diagnosis and management of clear cell acanthoma.
What Are the Characteristic Features of Dermoscopy in Clear Cell Acanthoma?
Clear Cell Acanthoma (CCA) exhibits some characteristic features under dermoscopic examination that help physicians make accurate diagnoses. The following are typical dermoscopic features of CCA:
Cobblestone-like surface: The lesion surface appears as uniform granular structures similar to cobblestones.
Regular dotted or comma-shaped vessels: Vessels are evenly distributed, regular in shape, usually appearing red or purple.
Well-defined borders: Clear boundaries between the lesion and surrounding normal skin, with regular edges.
Absence of pigmentation: CCA typically lacks melanin pigmentation, which contrasts sharply with certain malignant skin lesions.
These characteristic features make dermoscopic examination an important tool for diagnosing CCA.
How to Differentiate Clear Cell Acanthoma from Other Skin Lesions Using Dermoscopy?
Clear cell acanthoma dermoscopy needs to be differentiated from other common skin lesions. Here are some key points:
Differentiation from seborrheic keratosis: Seborrheic keratosis typically presents with a "brain-like" surface structure and cornified plugs, while CCA presents with a cobblestone-like surface and regular vessels.
Differentiation from basal cell carcinoma: Basal cell carcinoma commonly shows arborizing vessels and ulceration under dermoscopy, while CCA has more regular vascular morphology without ulceration.
Differentiation from melanoma: Melanoma typically presents with irregular pigmentation and polymorphic vessels, while CCA lacks pigmentation and has regular vascular morphology.
Through dermoscopic examination, physicians can more accurately differentiate CCA from other skin lesions, reducing the possibility of misdiagnosis.
Why is Dermoscopy Important for Early Detection of Clear Cell Acanthoma?
Dermoscopic examination is significant for the early detection of clear cell acanthoma. Early CCA may present as subtle erythema or papules that are easily overlooked or misdiagnosed. Through dermoscopy, physicians can observe subtle lesion features, such as a cobblestone-like surface and regular vessels, making a diagnosis at an early stage. Early detection not only facilitates timely treatment but also avoids unnecessary biopsies and surgeries.
What Are the Precautions for Using Dermoscopy in Clear Cell Acanthoma?
When using dermoscopy to examine clear cell acanthoma, the following precautions should be noted:
1. Clean the lesion area: Ensure the skin surface is free of oils or dirt to obtain clear images.
2. Select appropriate dermoscope: Choose a handheld or desktop dermoscope based on the location and size of the lesion.
3. Properly use coupling agent: Apply a coupling agent (such as alcohol or gel) to the lesion area to reduce skin surface reflection.
4. Avoid excessive pressure: Avoid pressing the lesion area too hard during examination to prevent affecting vascular morphology observation.
5. Combine clinical experience: Dermoscopic examination results need to be integrated with the physician's clinical experience for comprehensive judgment, avoiding sole reliance on images.
Following these precautions can improve the accuracy and reliability of dermoscopic examinations.
How to Maintain and Care for Dermoscopy Equipment Used in Clear Cell Acanthoma Examination?
Maintenance and care of dermoscopic equipment are crucial to ensuring the accuracy of examination results. Here are steps for equipment maintenance:
1. Regular lens cleaning: Use specialized lens cleaning cloths and solutions to regularly clean the dermoscope lens, avoiding dust and dirt affecting image quality.
2. Check light source: Ensure the dermoscope's light source works properly, replacing bulbs or batteries when necessary.
3. Avoid collisions and drops: Dermoscopes are precision instruments and should be protected from impacts and drops to prevent damage to internal components.
4. Storage environment: Store the dermoscope in a dry, clean environment, avoiding high temperatures and humidity.
5. Regular calibration: Periodically send the dermoscope to professional institutions for calibration to ensure imaging accuracy.
By following these steps, the dermoscope's lifespan can be extended, ensuring its accuracy in clear cell acanthoma examinations.
What Are the Latest Research Advances in Dermoscopy for Clear Cell Acanthoma?
In recent years, significant progress has been made in clear cell acanthoma dermoscopy research. The following are some of the latest research findings:
Application of high-resolution dermoscopy: High-resolution dermoscopy can more clearly display the fine structures of CCA, such as vascular morphology and surface texture, improving diagnostic accuracy.
AI-assisted diagnosis: Some studies attempt to apply artificial intelligence (AI) technology to dermoscopic image analysis, automatically identifying CCA features through machine learning algorithms to reduce human error.
Combination of new imaging technologies: Combining optical coherence tomography (OCT) with dermoscopy provides deeper lesion information, helping differentiate CCA from other skin lesions.
These research advances offer new possibilities for early diagnosis and precise treatment of CCA.
How Can Dermoscopy Be Used in Follow-Up Observation of Clear Cell Acanthoma?
Dermoscopic technology has important applications in the follow-up observation of clear cell acanthoma. Here are its specific roles in follow-up:
Monitoring lesion changes: Through regular dermoscopic examinations, physicians can observe changes in CCA size, color, and vascular patterns, evaluating whether the lesion is stable or progressing.
Evaluating treatment effectiveness: After treatment, dermoscopy can be used to check whether the lesion has completely resolved or recurred, helping adjust treatment plans.
Reducing unnecessary biopsies: For stable CCA, dermoscopic examination can avoid frequent biopsies, reducing patient discomfort and economic burden.
Through dermoscopic follow-up, physicians can more comprehensively understand the dynamic changes of CCA and develop personalized management strategies.
How to Analyze and Interpret Typical Dermoscopic Images of Clear Cell Acanthoma?
Analysis of clear cell acanthoma dermoscopic images requires attention to several key features:
1. Surface structure: Observe whether the lesion presents a typical "cobblestone-like" surface, which is an important feature of CCA.
2. Vascular pattern: Note the morphology and distribution of vessels; CCA typically presents with regular dotted or comma-shaped vessels.
3. Border clarity: CCA borders are usually clear and regular, contrasting sharply with surrounding normal skin.
4. Pigmentation: CCA typically lacks pigmentation, differing from certain malignant lesions.
By systematically analyzing these features, physicians can more accurately interpret CCA dermoscopic images and make correct diagnoses.
How Can Primary Care Institutions Implement Dermoscopy Screening for Clear Cell Acanthoma?
Primary care institutions can implement clear cell acanthoma dermoscopy screening following these steps:
1. Equipment procurement and training: Purchase appropriate dermoscopic equipment and provide professional training for medical staff, ensuring they master basic dermoscope operation and image interpretation skills.
2. Develop screening processes: Based on local conditions, establish CCA screening processes, including target populations, examination frequency, and follow-up plans.
3. Patient education: Educate patients about CCA through promotional materials or health lectures, increasing their willingness to participate in screening.
4. Establish referral mechanisms: Promptly refer suspected CCA cases to higher-level medical institutions for further examination and treatment.
Through these measures, primary care institutions can effectively implement dermoscopic screening for CCA, improving early diagnosis rates.
What Are the Skin Preparation and Patient Education Steps Before Dermoscopy for Clear Cell Acanthoma?
Skin preparation and patient education are important aspects of ensuring smooth clear cell acanthoma dermoscopy examinations. Here are the specific steps:
1. Skin cleaning: Guide patients to clean the lesion area, removing oils and dirt to obtain clear dermoscopic images.
2. Avoid cosmetics: Advise patients to avoid using cosmetics or skincare products before examination to prevent affecting examination results.
3. Explain the examination process: Explain to patients in detail the purpose, steps, and possible sensations of dermoscopic examination to reduce anxiety.
4. Sign informed consent: Ensure patients sign informed consent forms for cases requiring application of coupling agents or other special procedures.
5. Provide post-examination care advice: Inform patients of post-examination precautions, such as keeping the skin clean and avoiding friction.
Through thorough skin preparation and patient education, the accuracy of dermoscopic examinations and patient compliance can be improved.
Clear Cell Acanthoma (CCA) is a benign but easily misdiagnosed skin tumor. Clear cell acanthoma dermoscopy, with its non-invasive and high-resolution advantages, has become an important tool for CCA diagnosis and follow-up. This article details the working principles of dermoscopic examination, typical features (such as cobblestone-like surface and regular vascular patterns), and its applications in differential diagnosis, early detection, and treatment monitoring. Additionally, the article discusses the limitations of dermoscopic examination, equipment maintenance methods, and how primary care institutions can implement CCA screening. By combining the latest research advances and practical application cases, this article provides comprehensive guidance for dermatologists and healthcare practitioners, aiming to improve diagnostic accuracy and patient management of CCA.