Article
Dermatoscope for Dermatology
Dermoscopy, also known as epidermal transillumination microscopy, is a non-invasive, fast and easy means of examining the skin, which has a wide range of applications and plays an important role especially in different areas of dermatology. Dermoscopy has significant advantages in the diagnosis of skin tumours. By observing the pigmentation, blood vessels, texture and other…
Dermoscopy, also known as epidermal transillumination microscopy, is a non-invasive, fast and easy means of examining the skin, which has a wide range of applications and plays an important role especially in different areas of dermatology. Dermoscopy has significant advantages in the diagnosis of skin tumours. By observing the pigmentation, blood vessels, texture and other features of the skin surface, doctors can make preliminary judgement on the goodness or badness of the tumour; by analysing the inflammatory manifestations of the skin such as erythema, oedema, and pustules through the dermoscopy, doctors can diagnose a wide range of inflammatory skin diseases, such as psoriasis, eczema, and so on. Dermoscopy can also assist in the observation and diagnosis of hair diseases, nail diseases and vascular diseases.

The Role of Dermoscopy in the Diagnosis of Skin Cancer
Melanoma is a highly malignant tumour and early detection and treatment is essential to improve patient survival. By magnifying the surface of the skin 10 to 20 times, dermoscopy is able to clearly show the fine structures of melanoma, such as irregular pigment networks or abnormal blood vessel patterns. These features are important in differentiating melanoma from other benign lesions.
Non-melanoma skin cancers mainly include the types of squamous cell carcinoma and basal cell carcinoma. These skin cancers usually show symptoms such as gradual enlargement of skin lesions, rough or scaly surface, uneven colour, bleeding or discharge, and painless ulcers.
Dermoscopy can assist the doctor in determining the benign or malignant nature of the lesion. Malignant lesions usually have abnormal morphological features, such as cellular anisotropy and increased nuclear division, whereas benign lesions usually have good cellular differentiation and cellular morphology similar to that of normal tissue.

Dermoscopy in Inflammatory Skin Diseases
Psoriasis is a common inflammatory skin disease, which is characterised dermoscopically by evenly distributed punctate, globular, circumscribed or hairpin-like blood vessels on a bright red background with diffuse white scales. Eczema is an inflammatory skin reaction with intense itching caused by a variety of internal and external factors. Under dermoscopy, the features of eczema include small flakes or fine dots of bleeding, follicular papules, oozing, and crusting.
Dermoscopy can also be used to diagnose a variety of other inflammatory skin conditions, such as pityriasis rosea and lichen planus. Pityriasis rosea presents with peripheral white scales on a yellow background (collar sign) and clustered distribution of punctate blood vessels. Lichen planus shows pearly white, yellow or bluish-white Wickham’s stripe, which may be reticular in form.
The Role of Dermoscopy in the Diagnosis of Vascular Lesions
For specific types of vascular tumours, such as spider nevus or capillary dilatation, there are typical morphological features in dermoscopy. For example, a spider nevus may present dermoscopically with a small red spot in the centre, surrounded by many tiny red blood filaments radiating in the shape of a spider’s web. Through dermoscopy, the doctor can also clearly observe the morphology and distribution of capillaries, so as to assess the degree and extent of capillary dilatation.
Dermoscopy also plays an important role in the differential diagnosis of vascular tumours. Vascular tumours include various types, such as hemangiomas and angiofibromas. Angiofibromas appear dermoscopically as nodules or masses on the skin surface with well-defined borders.

The Use of Dermoscopy in Dermatological Treatments
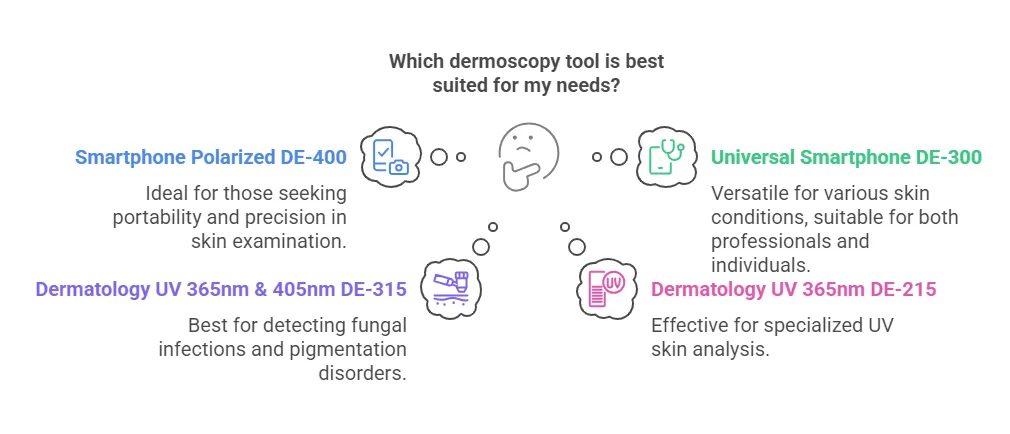
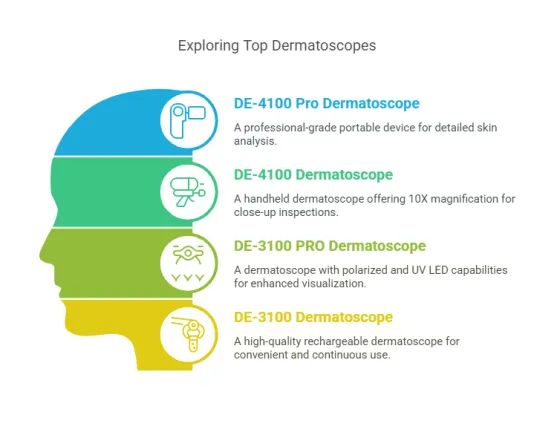
IBOOLO, as a professional dermatoscope brand, has launched different series of dermatoscopes to meet the requirements of different groups of people, and DE-3100 and DE-4100, as the high-end optical dermatoscopes of IBOOLO, play an important role in dermatological treatments, especially for the evaluation and planning of the treatment results.
IBOOLO dermatoscopes can reflect the colour and structural characteristics of the epidermis and dermal papillary layer by means of the optical magnification principle, thus assisting in the diagnosis of a wide range of skin diseases. By urging patients to have regular dermoscopy examinations, doctors can achieve dynamic follow-up of skin damage. In this process, doctors can readily determine the effectiveness of treatment and adjust the treatment plan according to changes in the condition. For example, in chloasma treatment, a skin image analysis system can be used to analyse the dermoscopic images and calculate the degree of regression and colour change of the pigmented area after treatment to determine the efficacy of the treatment.

Standardised Procedure for Dermoscopy
If you would like to use the IBOOLO Dermatoscope to perform a dermatoscopic examination, then take a look at the tutorial below.
When choosing an IBOOLO dermatoscope for a full-body skin examination, first clean the surface of the skin to be examined, removing oil, make-up, and other reflective substances. Disinfect the dermatoscope lens and other examination instruments to ensure sterility. Beginning with the head, gradually work your way down to examine the skin of the entire body, noting the condition of the skin in each area. For large skin areas, a zonal examination method can be used to avoid missing them. If a dermoscopic examination of a specific area is desired, the process is the same.
Another major point of interest during the examination is focusing and choosing the distance at which to look. both the DE-3100 and DE-4100 dermatoscopes can be used either close to the skin or at a distance from the area under observation. For patients with ulcerated or inflamed lesions, the latter may be more appropriate. This provides maximum comfort for the patient.
Both the DE-3100 and DE-4100 models can be connected to a mobile phone, which makes it possible to save dermatoscopic images with the mobile phone camera. By comparing dermatoscopic images on a regular basis, the doctor can visualise the changes in the lesions and make a more rational treatment plan.
Dermatoscope for Dermatology: How Dermatoscopy Revolutionizes Skin Care - IBOOLO
Explore how dermatoscopy and dermatoscope for dermatology enhance medical care through precise diagnostics, from early skin cancer detection to cosmetic assessment, revolutionizing examination through portable devices and AI integration.
Dermatoscopy in Dermatology: A Comprehensive Analysis from Diagnosis to Telemedicine
Dermatoscopy, as a revolutionary tool in dermatology, is transforming how physicians diagnose and treat skin diseases. Through high magnification and advanced light source technology, dermatoscopes reveal microscopic skin structures that are difficult to detect with the naked eye, significantly improving early diagnosis rates for skin cancer and other conditions. Moreover, dermatoscopy plays a crucial role in telemedicine, cosmetic dermatology, and healthcare in resource-limited regions. This article explores the working principles of dermatoscopy, its applications, and its profound impact on the future of dermatology.
What is a Dermatoscope? An Introductory Guide to Dermatological Tools
A dermatoscope is a specialized tool used for dermatological examinations, primarily for observing microscopic structures on the skin's surface. It helps physicians see details in the epidermal layers more clearly through high magnification and special light sources (such as polarized light). The core function of dermatoscopy is to assist in diagnosing skin diseases, especially early screening for skin cancer.
Working Principle: Dermatoscopes magnify the skin's surface and reduce light reflection, allowing physicians to observe pigment distribution and vascular structures that are difficult to detect with the naked eye.
Suitable Scenarios: Commonly used for preliminary diagnosis of melanoma, basal cell carcinoma, and other skin lesions.
Tool Components: Typically includes a magnifying lens, light source (LED or halogen), and polarizing filters.
The advent of dermatoscopy has fundamentally changed how dermatologists diagnose conditions, enabling them to identify potential problems earlier and more accurately.
The Evolution of Dermatoscopy in Skin Care
Since its introduction in the 1980s, dermatoscopy has undergone several major improvements. Initially, dermatoscopes were only used to study pigmented lesions, but as technology advanced, their application range gradually expanded.
Early Stage: Dermatoscopy was primarily used for preliminary screening of melanoma, with relatively limited functionality.
Technological Progress: Modern dermatoscopes are equipped with high-definition cameras, digital imaging systems, and AI-assisted diagnostic capabilities, significantly enhancing diagnostic efficiency.
Application Extension: Besides skin cancer screening, dermatoscopy is now used to diagnose common skin conditions such as eczema and psoriasis.
The evolution of dermatoscopy has not only improved diagnostic accuracy but also provided patients with earlier treatment opportunities.
How Does Dermatoscopy Improve the Accuracy of Skin Cancer Detection?
The role of dermatoscopy in skin cancer detection cannot be overlooked, especially in the early diagnosis of melanoma. Here's how dermatoscopy enhances detection accuracy:
1. Step 1: Magnified observation - dermatoscopes provide 10x to 20x magnification, helping physicians see minute changes in the skin's surface layers.
2. Step 2: Reduced light interference - polarized light technology reduces reflection from the skin's surface, allowing physicians to observe deeper pigment and vascular structures.
3. Step 3: Recording and analysis - modern dermatoscopes are equipped with digital imaging systems that can record changes in lesion areas for subsequent tracking and analysis.
Through these steps, dermatoscopy significantly increases the early detection rate of skin cancer, giving patients valuable treatment time.
What Are the Key Features of Modern Dermatoscopes?
When choosing a suitable dermatoscope, several key features need to be considered:
Magnification: Typically 10x to 20x, enabling clear observation of microscopic skin structures.
Light Source Type: LED light sources are energy-efficient and long-lasting, while halogen lamps provide more natural colour rendering.
Polarized Light Function: Reduces reflection from the skin's surface, enhancing the visibility of deeper structures.
Portability: Lightweight design facilitates use in different scenarios.
Digital Imaging: Supports high-definition image capture and storage for subsequent analysis and patient education.
These features collectively determine the performance and user experience of dermatoscopes, and selection should be based on actual needs.
What Advantages Does Dermatoscopy Have Compared to Traditional Skin Examination Methods?
Traditional skin examinations mainly rely on visual observation and palpation, while dermatoscopy provides more comprehensive diagnostic information through technological means. Here's a comparison:
Accuracy: Dermatoscopy can observe microscopic structures invisible to the naked eye, significantly improving diagnostic accuracy.
Efficiency: Dermatoscopy can be completed in minutes, while traditional methods may require multiple follow-up visits.
Patient Experience: Dermatoscopy requires no invasive procedures, reducing patient discomfort.
Data Recording: Modern dermatoscopes support image storage, facilitating long-term tracking and condition analysis.
Compared to traditional methods, dermatoscopy has clear advantages in terms of accuracy, efficiency, and patient experience, making it an essential tool in dermatological diagnosis.
What is the Role of Dermatoscopy in Teledermatology?
With the popularization of telemedicine, dermatoscopy is becoming increasingly widespread in teledermatology. Through high-definition imaging and digital transmission technology, dermatoscopes enable physicians to remotely analyze patients' skin conditions.
Remote Diagnosis: High-definition images captured by dermatoscopes can be transmitted over networks to specialists, helping patients in remote areas receive professional diagnoses.
Real-time Consultation: Physicians can provide real-time advice to patients through video calls combined with dermatoscopic images.
Case Storage: Dermatoscopic images can be archived for subsequent tracking and condition comparisons.
The remote application of dermatoscopy not only improves the accessibility of medical resources but also saves patients time and costs.
How Do Dermatologists Master Dermatoscopy Skills?
Dermatoscopy is a skill that requires professional training and experience. Here are the key steps for dermatologists to master dermatoscopy:
1. Step 1: Theoretical learning - study the basic principles of dermatoscopy, usage methods, and characteristics of common skin lesions.
2. Step 2: Practical operation - perform actual operations under mentor guidance, becoming familiar with equipment use and image interpretation.
3. Step 3: Case accumulation - enhance diagnostic accuracy and speed by analyzing numerous clinical cases.
4. Step 4: Continuous learning - participate in professional training and academic conferences to understand the latest technologies and research findings.
Mastering dermatoscopy skills takes time and practice, but it can significantly enhance diagnostic capabilities.
Which Common Skin Diseases Can Dermatoscopy Diagnose?
Dermatoscopy plays an important role in the diagnosis of various skin diseases. Here are some common examples:
Basal Cell Carcinoma: Dermatoscopy helps identify typical vascular patterns and pigment distribution.
Psoriasis: Assists in diagnosis by observing skin surface scales and vascular morphology.
Pigmented Lesions: Such as melanoma, dermatoscopy clearly shows pigment distribution and structural features.
Eczema: Dermatoscopy can observe minute inflammatory changes in the skin's surface layers.
The versatility of dermatoscopy makes it an important tool for dermatologists.
How Are Artificial Intelligence and Technology Shaping the Future of Dermatoscopy?
Artificial Intelligence (AI) and new technologies are bringing revolutionary changes to dermatoscopy:
AI-Assisted Diagnosis: Through machine learning algorithms, AI can quickly analyze dermatoscopic images and provide diagnostic suggestions.
Image Enhancement Technology: New imaging technologies can further improve image clarity and detail presentation.
Remote Collaboration: Combined with 5G technology, dermatoscopy can achieve real-time remote collaboration and diagnosis.
Data Integration: AI can combine dermatoscopic data with patient history to provide personalized diagnostic solutions.
In the future, dermatoscopy will become more intelligent and precise, bringing more convenience to patients and physicians.
How Can Dermatologists Maximize the Use of Dermatoscopy in Practice?
Here are some practical suggestions to help dermatologists better utilize dermatoscopes:
Regular Equipment Calibration: Ensure that the dermatoscope's magnification and light source are in optimal condition.
Establish an Image Library: Archive images of typical cases for teaching and reference.
Combine Clinical Experience: Combine dermatoscopy results with patients' clinical symptoms to improve diagnostic accuracy.
Patient Education: Use dermatoscopic images to explain conditions to patients, enhancing their understanding and cooperation.
Team Collaboration: Share dermatoscopic data with other departments to improve comprehensive medical treatment levels.
By optimizing usage methods, dermatoscopy can become a powerful assistant for dermatologists.
How Are Portable Dermatoscopes Revolutionizing Mobile Diagnosis?
Portable dermatoscopes, with their lightweight and user-friendly features, are changing how dermatologists diagnose conditions. Here are their advantages and application scenarios:
Anytime, Anywhere Diagnosis: Portable dermatoscopes are suitable for use in clinics, hospitals, or even outdoors, allowing physicians to quickly examine patients' skin conditions.
Efficient and Convenient: Requiring no complex setup, they can be used immediately after powering on, particularly suitable for emergency or rapid screening scenarios.
Patient-Friendly: The lightweight design reduces patient anxiety, improving the examination experience.
Portable dermatoscopes not only improve diagnostic efficiency but also provide physicians with greater flexibility.
Why Can Dermatoscopy Enhance Patient Trust and Understanding?
Dermatoscopy significantly enhances patient trust and engagement through intuitive image display:
1. Step 1: Visualization Diagnosis
Dermatoscopic images clearly show skin problems, helping patients understand their conditions more intuitively.
2. Step 2: Transparent Communication
Physicians can use images to explain lesion characteristics to patients, reducing information asymmetry.
3. Step 3: Confidence Building
After seeing clear diagnostic evidence, patients have more confidence in treatment plans.
Dermatoscopy is not just a diagnostic tool but also a bridge for physician-patient communication.
What Are the Applications of Dermatoscopy in Cosmetic Dermatology?
Besides medical diagnosis, dermatoscopy also plays an important role in cosmetic dermatology:
Skin Aging Assessment: By observing skin texture and pigment distribution, dermatoscopy helps evaluate ageing levels and develop personalized care plans.
Pigmentation Analysis: Dermatoscopy clearly shows the depth and range of pigmentation, helping select appropriate whitening treatments.
Scar Repair Monitoring: Track microscopic changes during the scar repair process to optimize treatment effects.
Dermatoscopy provides a scientific basis for cosmetic dermatology, enhancing treatment precision.
Is Investing in a Dermatoscope Worthwhile?
For dermatology clinics, purchasing a dermatoscope is an important investment decision. Here's an analysis of costs and value:
Initial Cost: High-end dermatoscopes are relatively expensive, but long-term use can improve diagnostic efficiency and accuracy.
Patient Attraction: Clinics equipped with dermatoscopes are more competitive and can attract more patients.
Diagnostic Benefits: Early detection of diseases such as skin cancer can save patients substantial treatment costs.
Brand Image: Advanced equipment enhances the clinic's professional image, strengthening patient trust.
Overall, the return on investment for dermatoscopes is relatively high, making them a wise choice for dermatology clinics.
How Does Dermatoscopy Improve Skin Care in Resource-Limited Regions?
Dermatoscopy is playing an important role in resource-limited or remote areas:
Remote Diagnostic Support: Through images captured by dermatoscopes, physicians in remote areas can receive guidance from specialists.
Low-Cost Screening: Portable dermatoscopes are relatively affordable and suitable for regions with limited resources.
Improved Medical Standards: Dermatoscopes help local physicians enhance their diagnostic capabilities, reducing misdiagnoses and missed diagnoses.
The popularization of dermatoscopy brings more equitable medical opportunities to resource-limited regions.
Through high magnification and polarized light technology, dermatoscopes provide dermatologists with clearer views of microscopic skin structures, significantly improving the accuracy of skin disease diagnosis, especially in early screening for skin cancer. As technology advances, the application range of dermatoscopy continues to expand, extending from traditional medical diagnosis to cosmetic dermatology and telemedicine. The emergence of portable dermatoscopes has further revolutionized mobile diagnosis, allowing physicians to conduct examinations anytime and anywhere. Additionally, the popularization of dermatoscopy in resource-limited regions provides patients in remote areas with more equitable medical opportunities. In the future, with the integration of artificial intelligence and digital imaging technology, dermatoscopy will become more intelligent and precise, bringing more convenience and value to dermatologists and patients.