Article
Dermascope Skin Analysis
Through dermoscopy, physicians are able to visualize slight alterations in the skin, such as blood vessels and pigmentation. It is first used for the screening of skin tumours, for the diagnosis of skin infections and inflammatory diseases, and for the monitoring of vascular skin lesions. This article provides a brief outlook on the application and…
Through dermoscopy, physicians are able to visualize slight alterations in the skin, such as blood vessels and pigmentation. It is first used for the screening of skin tumours, for the diagnosis of skin infections and inflammatory diseases, and for the monitoring of vascular skin lesions. This article provides a brief outlook on the application and effectiveness of dermoscopy. This article is helpful for readers to the know basic principles of how to use dermatoscopes correctly.
Introduction to Dermoscopy Examination
Dermoscopy is the use of a dermascope by a doctor to examine the skin of a patient. It needs only the full exposure of the examination area and no special preoperative preparation. For example, IBOOLO Dermatoscope is used to distinguish between benign pigmented nevi and malignant melanomas and to check for abnormal growth or malignancy.

Preparation for Dermoscopy
The patient will need to clean the skin prior to the examination, removing oils, dirt, make-up, hand-held patients. etc., dermatoscope, The so the examination that dermatoscope room the probe needs physician is to can first be clearly sterilised well visualise to lit the avoid so skin cross-infection that condition. between the Before doctor using can the clearly observe the skin condition. At the same time, the doctor needs to adjust the light and focus according to the observation needs.
Dermoscopy-related Equipment and Tools
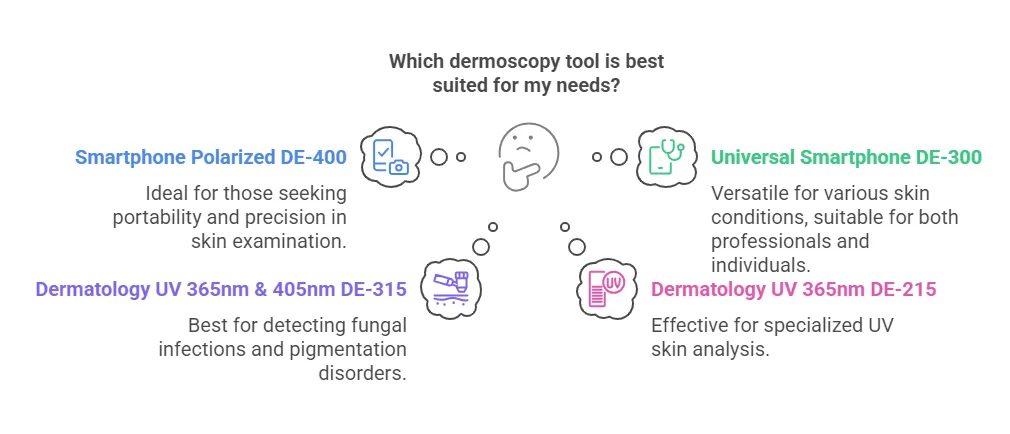
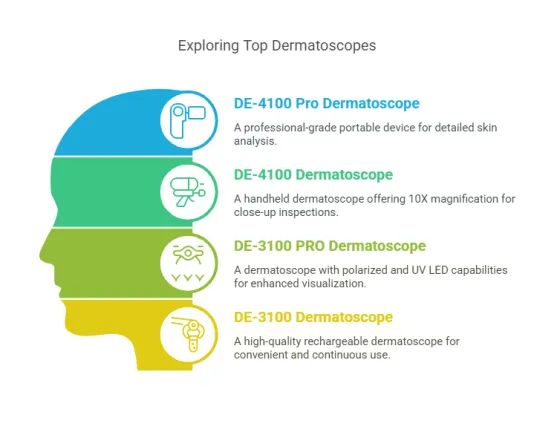
Dermascopes can be broadly categorised into digital dermoscopes and handheld dermoscopes. Handheld dermatoscopes are the most traditional and common type of dermatoscopy equipment. The DE-3100 and DE-4100 are part of IBOOLO’s professional handheld dermatoscopy series, with a magnification of 10X and four built-in different illumination modes.
IBOOLO dermascope devices are now designed to be used with smartphone accessories. Examples include cases with threads as well as universal phone clips and magnetic rings. Users can use them with the accessories and save dermascope images through their mobile phones.

Steps in Dermoscopy
Prior to the dermoscopic examination, the patient will keep the area of skin under observation clean. The doctor should point the dermatoscope’s probe at the area to be examined, select the appropriate illumination mode and adjust the focus until the image is clear enough for observation.IBOOLO handheld dermatoscopes are packaged by default with a mobile phone clip and a magnetic ring, which allows the user to connect the dermatoscope to a mobile phone for image saving.
Analysis of Dermoscopic Images
Colour is one of the most visual and important features of a dermoscopic image, with different colours reflecting the depth, nature and composition of the skin lesion. Brown and black colours are usually associated with the distribution of melanin within the epidermis. Blue or grey, on the other hand, suggests that melanin is located in the dermis and is a potential marker of malignant melanoma.
Patterns are structural features in dermoscopic images that reflect the histological properties of a skin lesion, such as reticular patterns. Brown or black reticular structures are commonly found in benign nevi. Irregularities, fractures or thickening of the reticulation may indicate malignant lesions.
Structural analysis focuses on the borders, shape, and internal structure of the skin lesion. Benign lesions have clear, smooth borders. Malignant lesions often present fuzzy, irregular borders. Uniform structure is usually a sign of a benign lesion. Uneven, disorganised structures suggest malignant potential.
Dermoscopic image analysis can assist the physician in the early identification of malignant lesions such as melanoma, basal cell carcinoma, and squamous cell carcinoma by providing a detailed view of the colours, patterns, and structures. Dermoscopy improves diagnostic sensitivity and specificity compared to visual observation.

Clinical Significance of Dermatological Microscopy
Through dermoscopy, doctors can distinguish between harmless and dangerous skin growths and enhance the diagnostic precision, rate which for may early decrease stage the melanoma chances can of be misdiagnosis 90% or or underdiagnosis. better, The while five the year survival survival rate for advanced melanoma is significantly worse. Other skin cancers are also highly curable if treated surgically at an early stage with a cure rate of nearly 100%.
Limitations and Challenges of Dermoscopy
This is because dermoscopy enhances the early diagnosis precision through magnification of skin features and visualization of the skin surface and its superficial structures in comparison to the conventional visual assessments. Compared to other techniques, imaging such as skin ultrasound and optical coherence tomography, it has the advantages of being portable, relatively to cheap, display and information easy from to deeper use. tissues, However, and it having has specific the and disadvantages sensitive of signals being that operator are dependent, determined unable by optical methods. These issues can be solved by increasing the level of training of physicians, incorporating other diagnostic methods (biopsy and ultrasound), and enhancing the equipment technology, which may include higher resolution and multimodal imaging.

Future Developments in Dermoscopy
Future developments in dermoscopy are focused on technological progress and skill development. AI can enhance the ability of doctors to analyze dermoscopy images quickly and accurately, detect malignant lesions and decrease the probability of misdiagnosis. However, telemedicine and digital technologies are also expanding the front door of the doctor’s office to the internet, enabling image sharing, specialist cooperation, and tele-diagnosis, especially in areas with limited access to healthcare providers. To fully take advantage of these technologies, doctors will need to resources continue and to gaining develop hands-on their experience. skills, The for use instance of by technology attending and training specialisation sessions, will using increase the the internet role and of other electronic dermoscopy in diagnosis, prevention and management of health, thus making precision medicine available to more people.
Dermoscopy and Skin Health Management
Dermoscopy is a non-invasive, rapid and highly effective tool for the evaluation of skin lesions. It can help physicians differentiate between benign and malignant skin lesions and is especially important in the early detection of malignant tumours such as melanoma. In skin health monitoring, dermoscopy not only helps doctors to make an accurate diagnosis, but also provides a basis for ongoing follow-up and evaluation.
Dermascope Skin Analysis: Guide to Diagnosis & Monitoring - IBOOLO
Dermascope skin analysis helps diagnose and monitor skin conditions like melanoma and moles non-invasively. Learn key techniques, device selection, and best practices for accurate results. Ideal for dermatologists and patients.
Dermascope Skin Analysis: Key Technologies for Early Detection and Precision Diagnosis of Acral Melanoma and Beyond
Introduction to Dermascope Skin Analysis and Acral Melanoma
Acral melanoma, a highly aggressive form of skin cancer predominantly affecting the palms, soles, and nail beds, poses unique diagnostic challenges due to its atypical presentation and anatomical location. Early identification is critical to improving patient outcomes, and dermascope skin analysis has emerged as a cornerstone technology in this effort. By leveraging advanced optical imaging and artificial intelligence (AI), dermascope skin analysis enables clinicians to detect subtle malignant features—such as the "parallel ridge pattern" or "irregular streaks"—with a diagnostic accuracy of up to 89%, according to 2024 data from the International Dermoscopy Society (IDS). This article provides an in-depth exploration of the science behind dermascope skin analysis, its essential role in modern dermatology, and its evolving applications in both clinical and cosmetic settings, with a particular focus on acral melanoma.
The Science Behind Dermascope Skin Analysis
Dermascope skin analysis is grounded in the principles of optical imaging and microstructural analysis of the skin. This technology employs polarized light or immersion fluids to eliminate surface reflections from the stratum corneum, allowing for magnified visualization (10-40x) of features from the epidermis down to the dermal papillae. The core mechanisms include:
- Polarized Light Technology: By penetrating the epidermal layer and reducing light scatter, polarized light reveals intricate details of pigment distribution (e.g., melanin nests) and vascular patterns (e.g., tortuous vessels). This enhances the visibility of subsurface abnormalities critical for diagnosing conditions like acral melanoma.
- Multispectral Imaging: Advanced dermoscopes integrate infrared or ultraviolet light to highlight inflammation or deeper lesions, offering a multidimensional view of skin pathology.
- Morphological Algorithms: AI-driven analysis quantifies features such as pigment network symmetry, border regularity, and color variation—key parameters in the ABCD criteria (Asymmetry, Border, Color, Diameter)—to assess malignancy risk with precision.
According to IDS research from 2023, dermascope skin analysis boosts diagnostic specificity to 75%-90%, far surpassing the capabilities of naked-eye examination. This scientific foundation makes it an indispensable tool for early cancer detection and differential diagnosis.
Why Dermascope Skin Analysis Is Essential in Modern Dermatology
In contemporary dermatology, dermascope skin analysis is often described as the clinician’s “second pair of eyes,” offering unparalleled precision and versatility. Its clinical significance lies in several key areas:
1. Accurate Cancer Screening: Dermascope skin analysis excels at identifying early signs of melanoma (e.g., blue-white veil) and basal cell carcinoma (e.g., maple leaf-like areas), enabling timely intervention.
2. Reduced Misdiagnosis: By distinguishing benign conditions like seborrheic keratosis from malignant squamous cell carcinoma, it minimizes unnecessary treatments.
3. Dynamic Monitoring: Regular imaging tracks changes in moles or lesions over time, supporting risk stratification (e.g., Clark level classification).
4. Patient Empowerment: High-resolution images provide visual evidence of skin conditions, improving patient understanding and treatment adherence.
For acral melanoma, dermascope skin analysis is particularly vital due to the subtlety of its early features, such as diffuse pigment granules or fishbone-like vasculature, which are often missed by traditional methods.
Comparing Dermascope Technologies: Features and Trade-offs
Dermascope skin analysis encompasses a range of technologies, each tailored to specific clinical needs:
1. Polarized Light Dermoscopes (e.g., DermLite):
Advantages: Non-contact operation reduces infection risk and excels at visualizing deep vascular structures.
Limitations: Less effective for hyperkeratotic lesions due to reduced sensitivity to surface details.
2. Contact Dermoscopes (with Coupling Fluid):
Advantages: Eliminates surface glare, ideal for examining epidermal features like sweat pores.
Limitations: Time-consuming and prone to image instability from fluid application.
3. Digital Smart Dermoscopes (e.g., FotoFinder):
Advantages: Automated lesion annotation and cloud-based data comparison enhance diagnostic efficiency.
Limitations: High cost and reliance on regularly updated AI databases.
These variations ensure dermascope skin analysis can be adapted to diverse diagnostic scenarios, from routine screenings to complex cases like acral melanoma.
How Dermascope Skin Analysis Detects Early Skin Cancer
The process of detecting skin cancer via dermascope skin analysis is systematic and precise:
1. Preparation: The skin is cleaned to remove cosmetics or ointments that could obscure imaging.
2. Calibration: Light intensity is adjusted based on skin tone (Fitzpatrick scale) for optimal clarity.
3. Lesion Scanning:
- Assesses pigment network disruption or diffusion.
- Identifies hallmarks like the blue-white veil or crystalline structures (indicative of basal cell carcinoma).
- Evaluates vascular patterns (e.g., dotted or serpentine vessels suggesting malignancy).
4. Image Archiving: Records lesion coordinates, size, and features for longitudinal comparison.
For acral melanoma, dermascope skin analysis achieves a sensitivity exceeding 90% in early detection, with specificity above 80% for distinguishing benign nevi from suspicious lesions like Spitz nevi.
Scope and Limitations of Dermascope Skin Analysis
While dermascope skin analysis is highly versatile, its efficacy varies by lesion type:
- Pigmented Lesions: Focuses on pigment network uniformity (e.g., cobblestone pattern for benignity vs. radial streaming for malignancy).
- Non-Pigmented Lesions: Relies on vascular analysis (e.g., arborizing vessels in basal cell carcinoma).
- Inflammatory Conditions: Detects uniform dotted vessels in psoriasis or irregular erythema in eczema.
However, subcutaneous nodules (e.g., lipomas) require ultrasound, and advanced melanomas necessitate biopsy for confirmation, highlighting the tool’s role as a screening rather than definitive diagnostic method.
Dermascope Skin Analysis vs. Biopsy: Complementary Roles
Dermascope skin analysis does not replace biopsy but enhances its efficiency:
- Reduces Biopsy Rates: High negative predictive value (>95%) rules out low-risk lesions.
- Guides Targeted Biopsies: Pinpoints suspicious areas (e.g., color transition zones) for higher diagnostic yield.
- Non-Invasive Follow-Up: Monitors high-risk patients (e.g., those with multiple nevi syndrome) without repeated invasive procedures.
European guidelines recommend combining dermascope skin analysis with biopsy when lesions exceed 6mm, grow rapidly, or occur in patients with risk factors like family history or UV exposure.
The Vital Role of Dermascope Skin Analysis in Dermatology
Dermascope skin analysis is integral to global skin cancer screening protocols (e.g., AAD, EADO) due to its multidimensional diagnostic capabilities:
- Minimized Missed Diagnoses: Detects melanomas as small as 3mm with 91% sensitivity (British Journal of Dermatology, 2023).
- Optimized Treatment: Differentiates benign nevi from Spitz nevi, reducing unnecessary excisions by 28%.
- Quantitative Assessment: AI metrics (e.g., asymmetry index, color variance) refine risk stratification.
For acral melanoma, its non-invasive nature is especially valuable in sensitive areas like the palms and soles, where biopsy can be challenging.
Personalized Skin Analysis with Dermascope Technology
Dermascope skin analysis enables tailored diagnostics through a structured workflow:
1. Data Collection: Captures high-definition images of the epidermal-dermal junction using polarized light, measuring over 20 parameters (e.g., vascular density, pigment aggregation).
2. AI Interpretation: Matches findings against databases like PH2 or MED-NODE, generating risk scores (0-10) and visual reports (e.g., inflammation heatmaps).
3. Customized Plans:
- High-risk lesions: Recommends follow-up or biopsy within 3-6 months.
- Chronic dermatitis: Suggests anti-inflammatory agents like ceramides.
- Photoaging: Advises antioxidants (e.g., vitamins C/E) and sun protection.
This personalization enhances both clinical outcomes and patient satisfaction.
Long-Term Skin Health Monitoring with Dermascope Skin Analysis
Dermascope skin analysis supports ongoing skin health tracking in three key scenarios:
1. Pigmented Lesion Surveillance: Compares ABCD features every six months, flagging new vessels or structural distortions.
2. Treatment Efficacy: Quantifies changes in pore size or erythema post-acne therapy, or melanin activity in melasma patients.
3. Preventive Care: Annual screenings for high-risk groups (Fitzpatrick I-II) build a digital skin archive to monitor UV damage progression.
Devices require standardized color calibration and ≥20x optical zoom for consistent results, ensuring dermascope skin analysis remains a reliable long-term tool.
The Future of Dermascope Skin Analysis
Dermascope skin analysis represents a transformative leap in dermatology, blending cutting-edge imaging with AI to achieve unprecedented diagnostic precision. For acral melanoma, its ability to detect high-risk features like fishbone vasculature or diffuse pigment granules—coupled with 3D reconstruction to quantify lesion depth—offers a non-invasive alternative to traditional biopsy in early screening. While it excels at reducing missed diagnoses and guiding precise interventions, differential diagnosis with benign acral nevi or traumatic hemorrhage remains a challenge, necessitating histopathological confirmation for definitive results. Looking ahead, the integration of portable dermoscopes with cloud-based telemedicine platforms promises to enhance accessibility, particularly for underserved populations at risk of acral melanoma. As technology evolves, dermascope skin analysis will continue to redefine skin health management, bridging clinical excellence with personalized care.
Mastering Dermascope Skin Analysis: A Complete Guide for Accurate Diagnosis and Monitoring
Dermascope skin analysis is revolutionizing dermatology by providing a non-invasive, highly accurate method for diagnosing and monitoring skin conditions. From detecting early signs of melanoma to differentiating benign lesions, this technique combines magnification and advanced lighting to reveal hidden skin structures. Whether you're a dermatologist seeking to refine your diagnostic skills or a patient curious about self-examination, this guide covers everything from the basics of dermascope use to the latest advancements in AI and telemedicine. Learn how to interpret key patterns, choose the right device, and apply best practices for optimal skin health outcomes.
What is Dermascope Skin Analysis: A Comprehensive Guide for Beginners
Dermascope skin analysis is a non-invasive diagnostic technique used to examine skin lesions and conditions at a microscopic level. By magnifying the skin's surface, dermatologists can identify patterns, colors, and structures that are invisible to the naked eye. This method is particularly useful for detecting early signs of skin cancer, such as melanoma, and differentiating between benign and malignant lesions.
Why is it important?
Dermascope skin analysis enhances diagnostic accuracy, reducing the need for unnecessary biopsies. It also helps in monitoring skin conditions over time, ensuring timely intervention.
How does it work?
A dermascope uses polarized light and magnification to visualize the epidermis and dermis layers. This allows for detailed observation of pigmentation, vascular structures, and other key features.
Can beginners use it?
While professionals primarily use dermascopes, beginners can learn the basics through training and practice. Understanding common patterns like pigment networks and globules is a great starting point.
The Structure and Components of Modern Dermascopes for Skin Analysis
Modern dermascopes are sophisticated tools designed to provide clear, detailed images of the skin. Here’s a breakdown of their key components:
What are the main parts?
Magnification Lens: Typically offers 10x magnification for detailed viewing.
Light Source: Uses polarized or non-polarized light to illuminate the skin.
Contact Plate: A glass or plastic surface that touches the skin, often with gel for better clarity.
Camera Attachment: Allows for digital imaging and analysis.
Why does each component matter?
The combination of magnification and lighting helps reveal subtle skin structures, while the camera enables documentation and sharing of findings for further analysis.
How to choose the right dermascope?
Consider factors like portability, light type, and compatibility with digital tools for telemedicine or AI analysis.
Step-by-Step Workflow for Professional Dermascope Skin Analysis
Performing a professional dermascope skin analysis requires a systematic approach to ensure accuracy. Here’s a step-by-step guide:
1. Prepare the Patient:
- Clean the skin area to remove oils or debris.
- Apply a gel or alcohol to enhance visibility.
2. Set Up the Dermascope:
- Adjust the magnification and light settings based on the lesion type.
3. Examine the Lesion:
- Look for specific patterns like pigment networks, streaks, or vascular structures.
- Document findings using a camera attachment if available.
4. Analyze the Results:
- Compare the observed features with known dermoscopic criteria for diagnosis.
5. Plan Next Steps:
- Decide if a biopsy, monitoring, or treatment is necessary.
Working Principles of Digital Dermascopes: How They Analyze Skin Conditions
Digital dermascopes combine traditional dermoscopy with advanced technology for enhanced analysis.
How do they work?
Image Capture: High-resolution cameras take detailed photos of the skin.
Software Analysis: AI algorithms analyze the images, identifying patterns and potential abnormalities.
Data Storage: Images are stored for future reference and comparison.
Why are they better?
Digital dermascopes allow for remote consultations, second opinions, and long-term monitoring. They also reduce human error by providing AI-assisted insights.
Can they replace traditional methods?
While they enhance accuracy, they are best used alongside clinical expertise for a comprehensive diagnosis.
How to Use a Dermascope for Self-Skin Examination: A Guide for Patients
Patients can use handheld dermascopes for self-examination, especially if they have a history of skin conditions. Here’s how:
What do you need?
- A handheld dermascope with built-in lighting.
- A mirror or smartphone attachment for better viewing.
How to perform the examination:
1. Clean the skin area and apply a gel for clarity.
2. Place the dermascope against the skin and adjust the focus.
3. Look for unusual patterns, colors, or structures.
When to consult a doctor?
If you notice asymmetrical lesions, irregular borders, or changing patterns, seek professional advice immediately.
Why is self-examination helpful?
It empowers patients to monitor their skin regularly, catching potential issues early.
Clinical Applications of Dermascope Analysis in Dermatology Practice
Dermascope analysis has become an indispensable tool in dermatology, offering a non-invasive way to diagnose and monitor various skin conditions.
What conditions can it diagnose?
- Melanoma and other skin cancers.
- Benign lesions like moles, seborrheic keratosis, and Spitz nevi.
- Inflammatory conditions such as psoriasis and eczema.
Why is it preferred in clinical settings?
It reduces the need for unnecessary biopsies, provides real-time results, and enhances diagnostic accuracy through detailed visualization of skin structures.
How is it used in practice?
Dermatologists use dermascopes to:
- Identify early signs of melanoma using patterns like pigment networks and streaks.
- Monitor changes in lesions over time.
- Guide surgical procedures by mapping lesion borders.
Dermascope Analysis for Different Skin Types: Customizing Your Approach
Skin type plays a significant role in dermascope analysis, as pigmentation and texture vary across individuals.
Why does skin type matter?
- Darker skin tones may show different pigment patterns compared to lighter skin.
- Sensitivity to light and pressure varies, requiring adjustments in technique.
How to customize your approach:
For fair skin: Focus on vascular structures and subtle pigment changes.
For dark skin: Pay attention to blue-white veils and atypical patterns that may indicate malignancy.
For sensitive skin: Use minimal pressure and non-polarized light to avoid irritation.
Can one technique work for all skin types?
While the basic principles remain the same, adapting the approach based on skin type ensures more accurate and comfortable analysis.
Accuracy Rates of Dermascope Skin Analysis Compared to Biopsy Results
Dermascope analysis is highly accurate, but how does it compare to the gold standard of biopsy?
What do studies show?
- Dermascope analysis has an accuracy rate of 85-90% in diagnosing melanoma.
- When combined with clinical expertise, this rate increases significantly.
Why choose dermascopy over biopsy?
- It’s non-invasive and painless.
- It allows for immediate assessment and reduces patient anxiety.
How does it complement biopsy?
Dermascopy can help prioritize which lesions require biopsy, improving efficiency and reducing unnecessary procedures.
Can it replace biopsy entirely?
While highly accurate, biopsy remains essential for definitive diagnosis in uncertain cases.
4. Latest Features in Advanced Dermascopes for Enhanced Skin Analysis
Modern dermascopes come equipped with cutting-edge features that improve diagnostic capabilities.
What are the latest advancements?
AI Integration: Algorithms analyze images in real-time, providing diagnostic suggestions.
High-Resolution Cameras: Capture detailed images for better analysis and documentation.
Polarized and Non-Polarized Light Modes: Offer flexibility for different skin types and conditions.
Portable Designs: Handheld devices with wireless connectivity for telemedicine.
Why are these features important?
They enhance diagnostic accuracy, streamline workflows, and enable remote consultations.
How to choose the right features?
Consider your practice’s needs—whether it’s AI for faster analysis or portability for on-the-go use.
5. Choosing the Right Dermascope for Your Dermatology Practice: Quality Considerations
Selecting the right dermascope is crucial for effective skin analysis. Here’s what to consider:
What factors should you evaluate?
Magnification: 10x is standard, but higher magnification may be needed for specific cases.
Lighting: Polarized light reduces glare, while non-polarized light enhances surface details.
Ergonomics: Comfortable design for prolonged use.
Compatibility: Ability to integrate with digital systems or AI tools.
Why is quality important?
High-quality dermascopes provide clearer images, better durability, and more accurate results.
How to test before buying?
- Check image clarity and light consistency.
- Ensure ease of use and portability.
- Read reviews and consult peers for recommendations.
Can budget options be effective?
While budget-friendly models exist, investing in a high-quality dermascope ensures long-term reliability and better patient outcomes.
What are the Essential Precautions When Performing Dermascope Skin Analysis?
When conducting dermascope skin analysis, the first precaution is to ensure a clean skin surface. How do you achieve this? Gently cleanse the area to be examined with a mild, non - irritating cleanser. This step is crucial as dirt, oil, and cosmetics can interfere with the clarity of the dermascope image. For example, a thick layer of foundation might obscure important skin lesions.
Another key aspect is proper calibration of the dermascope. Why is calibration necessary? An uncalibrated dermascope can lead to inaccurate magnification and color representation. To calibrate, follow the manufacturer's instructions carefully. Usually, this involves adjusting the focus and white balance settings.
The operator should also wear appropriate protective gear. What kind of gear is requ
ired Gloves are essential to prevent cross - contamination between patients. Additionally, if the dermascope uses a light source that emits potentially harmful radiation, eye protection might be needed.
How to Maintain Your Dermascope in Optimal Condition?
Maintaining a dermascope starts with regular cleaning. Step by step, first, turn off the device. Then, use a soft, lint - free cloth slightly dampened with isopropyl alcohol to gently wipe the lens. Why is the lens cleaning important? A dirty lens can distort the image, making it difficult to accurately analyze the skin. After cleaning the lens, clean the body of the dermascope to remove any fingerprints or debris.
Storage is another vital factor. Where should you store your dermascope? Keep it in a protective case when not in use. This protects it from physical damage such as scratches or drops. The storage environment should be dry and away from direct sunlight. Exposure to moisture can cause internal components to corrode, and sunlight can fade the display or damage the light source.
Periodic professional servicing is also recommended. How often should this be done? Depending on the manufacturer's guidelines, it could be once a year or after a certain number of uses. During servicing, a technician will check for any loose parts, ensure the electrical components are functioning properly, and recalibrate the device if necessary.
Can Telemedicine and Dermascope Skin Analysis Enable Remote Diagnosis?
Telemedicine has opened up new possibilities for dermascope skin analysis. How does it work? A healthcare provider can use a dermascope to capture high - quality images of the patient's skin. These images can then be transmitted securely to a dermatologist or other specialist via a telemedicine platform. The specialist can review the images and provide a preliminary diagnosis.
Why is this beneficial? It increases access to dermatological expertise, especially in rural or remote areas where patients might not have easy access to a dermatologist. For example, a patient in a small town can receive a diagnosis from a renowned dermatologist in a big city without having to travel long distances.
However, there are limitations. What are they? The quality of the image transmitted can be affected by factors such as a poor internet connection. Also, the absence of physical examination might mean that some subtle skin features that can only be detected by touch are missed. Despite these limitations, with the continuous improvement of technology, telemedicine - enabled dermascope skin analysis has the potential to become an integral part of remote healthcare.
What are the Current Capabilities and Future Prospects of AI Integration in Dermascope Skin Analysis?
Currently, AI in dermascope skin analysis can assist in the identification of common skin lesions. How does it do this? AI algorithms are trained on a vast database of dermascope images. These algorithms can analyze the patterns, colors, and shapes in the images. For example, they can quickly distinguish between a benign mole and a potentially cancerous melanoma.
The current capabilities also include automated measurement of skin features. Why is this useful? It provides more accurate and consistent measurements compared to manual measurements. An AI - powered dermascope can measure the size of a lesion with high precision.
Looking into the future, AI integration is likely to improve diagnostic accuracy even further. How? As more data is collected and algorithms are refined, AI will be able to detect even the most subtle skin abnormalities. It might also be able to predict the progression of skin diseases. For example, in the case of psoriasis, AI could potentially predict when a flare - up is likely to occur based on changes in the skin over time.
What are the Training Requirements for Accurate Dermascope Skin Analysis Interpretation?
To accurately interpret dermascope skin analysis, a basic understanding of skin anatomy is essential. Why is this the starting point? Knowledge of the normal structure of the skin helps in identifying abnormal features. For example, understanding the normal distribution of blood vessels in the skin makes it easier to spot abnormal vascular patterns in certain skin conditions.
Training in image analysis techniques is also crucial. What kind of techniques are involved? This includes learning how to adjust the contrast and brightness of dermascope images to better visualize skin features. Operators should also be trained in pattern recognition. For example, they need to be able to recognize the characteristic "moth - eaten" appearance of a melanoma.
Hands - on experience is a significant part of the training. How much hands - on experience is required? A minimum of several dozen supervised cases is often recommended. During this time, trainees can practice interpreting images under the guidance of an experienced dermatologist. This hands - on experience allows them to become familiar with the nuances of different skin conditions as seen through a dermascope.
What Should You Look For in Dermascope Analysis for Early Skin Cancer Detection?
When using a dermascope for early skin cancer detection, one of the primary features to look for is asymmetry. Why is asymmetry important? Most normal moles are symmetric, while melanoma, a dangerous form of skin cancer, often shows an irregular shape where one half does not match the other. For example, if you draw a line through the center of a mole, and the two sides have different shapes, sizes, or patterns, it could be a warning sign.
Color variation is another crucial aspect. How does color indicate potential skin cancer? Normal moles typically have a uniform color, such as brown. However, in cases of skin cancer, multiple colors like black, brown, red, white, or blue may be present within a single lesion. A mole with a mix of these colors should be closely examined.
Border irregularity is also significant. What does an irregular border look like? An irregular border is ragged, notched, or blurred. In contrast, benign moles usually have smooth, well - defined borders. If a mole's border is not clearly defined and seems to blend unpredictably with the surrounding skin, it warrants further investigation.
How Do Handheld and Digital Dermascopes Compare for Comprehensive Skin Analysis?
When it comes to handheld dermascopes, they offer portability. Why is portability an advantage? They can be easily carried around, allowing dermatologists to perform skin analysis in various locations, including patients' bedsides or during home visits. Handheld dermascopes are also generally more affordable, making them accessible to a wider range of healthcare providers. However, they may have limitations in terms of image quality and data storage.
Digital dermascopes, on the other hand, provide high - resolution images. How do these high - resolution images benefit skin analysis? They can capture fine details that might be missed with a handheld device, enabling more accurate diagnosis. Digital dermascopes also often come with software for image enhancement and analysis. For example, the software can adjust the contrast and color balance of the image, highlighting subtle skin features. Additionally, they have the ability to store and manage large amounts of patient data, which is useful for tracking the progression of skin conditions over time.
How Are Portable Dermascopes Bringing Professional Skin Analysis to Remote Locations?
Portable dermascopes are revolutionizing skin analysis in remote areas. First, they are lightweight and easy to transport. Step by step, healthcare workers can simply pack the portable dermascope in a small bag and carry it to even the most isolated locations. For instance, in rural villages where there are no established dermatology clinics, a doctor can bring a portable dermascope during a mobile medical outreach.
These devices also often have long - lasting battery life. Why is this important? It allows for continuous use without the need for a constant power source, which may not be available in remote areas. Some portable dermascopes can operate for several hours on a single charge, ensuring that multiple patients can be examined during a visit.
Moreover, portable dermascopes are designed to be user - friendly. What does this mean for remote healthcare? Even healthcare providers with limited training in advanced dermatological equipment can quickly learn to use them. They usually have simple controls for focusing and capturing images, making it possible to perform basic skin analysis in remote locations where specialized training may be scarce.
What Are the Documentation Protocols for Dermascope Skin Analysis in Clinical Settings?
In clinical settings, accurate patient identification is the first step in documentation. Why is this crucial? All dermascope images and related data must be clearly associated with the correct patient to avoid mix - ups. This includes recording the patient's full name, date of birth, and unique patient identification number.
Next, a detailed description of the skin area being examined should be noted. What should this description include? It should specify the location on the body, such as the left shoulder or right thigh. The size, shape, and color of any skin lesions observed during the dermascope analysis should also be described. For example, "A 5 - mm, irregularly shaped, brown - black lesion was observed on the left forearm."
The images captured by the dermascope should be properly labeled. How? Include the patient's name, date of the examination, and a brief description of the area in the image file name. Additionally, the images should be stored in a secure, encrypted database to protect patient privacy. This ensures that the dermascope skin analysis data is organized, accessible, and compliant with privacy regulations.
How Can Patients Understand Their Dermascope Skin Analysis Results?
Healthcare providers should first explain the basic purpose of dermascope skin analysis to patients. Why is this important? Patients need to know that the analysis is used to detect and evaluate skin conditions, including potential skin cancers. They should be informed that the dermascope allows for a closer look at the skin's surface and subsurface structures.
When presenting the results, use simple and clear language. What kind of language should be used? Instead of medical jargon, explain findings in layman's terms. For example, if the result shows a "benign mole," tell the patient that it is a non - cancerous growth. If there are any areas of concern, describe them in a way that the patient can understand, such as "There is a spot on your skin that we want to keep an eye on because it has some unusual features."
Provide visual aids if possible. How can visual aids help? Show the patient the dermascope images and point out the relevant features. This can make it easier for them to grasp what the doctor is talking about. Additionally, offer written information or brochures about common skin conditions for the patient to review at home, further enhancing their understanding of the dermascope skin analysis results.
Dermascope skin analysis is a powerful tool in dermatology, enabling detailed examination of skin lesions and conditions without invasive procedures. This guide explores its clinical applications, from diagnosing melanoma to monitoring inflammatory conditions, and highlights the importance of adapting techniques for different skin types. It also delves into the accuracy of dermascopy compared to biopsies, the latest features in advanced devices, and how to choose the right dermascope for your practice. Additionally, the guide covers practical workflows, patient self-examination tips, and the role of AI and telemedicine in enhancing diagnostic capabilities. By understanding the principles and best practices of dermascope skin analysis, both professionals and patients can achieve better skin health outcomes.
Recommended reading
China-Based Dermascope Suppliers & Manufacturers Offers Affordable Design Services - IBOOLO
With over a decade of experience crafting tailored solutions, our China company suppliers & manufacturers high-quality affordable dermascopes to meet every customer's distinct requirements.
Wholesale Dermascope Vs Dermatoscopes Products Supply by Company in China - IBOOLO
We are a leading China-based dermascope vs dermatoscope products supply capable of providing wholesale lamps designed around our clients' specific needs. Our flexible products supply process ensures tailored solutions.
Dermascope vs Dermatoscope: Surpassing the Magnifying Glass - IBOOLO
IBOOLO: Dermascopes vs. Dermatoscopes - Surpassing the Limitations of the Magnifying Glass to Enable Precise Skin Evaluations and Enhanced Patient Outcomes