Article
Acral Melanoma Dermoscopy
Acral melanoma is a special subtype of skin cancer. Late presentation of patients and delayed diagnosis by doctors result in poor prognosis and survival. Despite advances in the understanding of the key features of this disease, early diagnosis of acral melanoma remains challenging. A combination of clinical presentation, dermoscopy, and histologic findings is essential for…
Acral Melanoma Dermoscopy: Early Detection Guide - IBOOLO
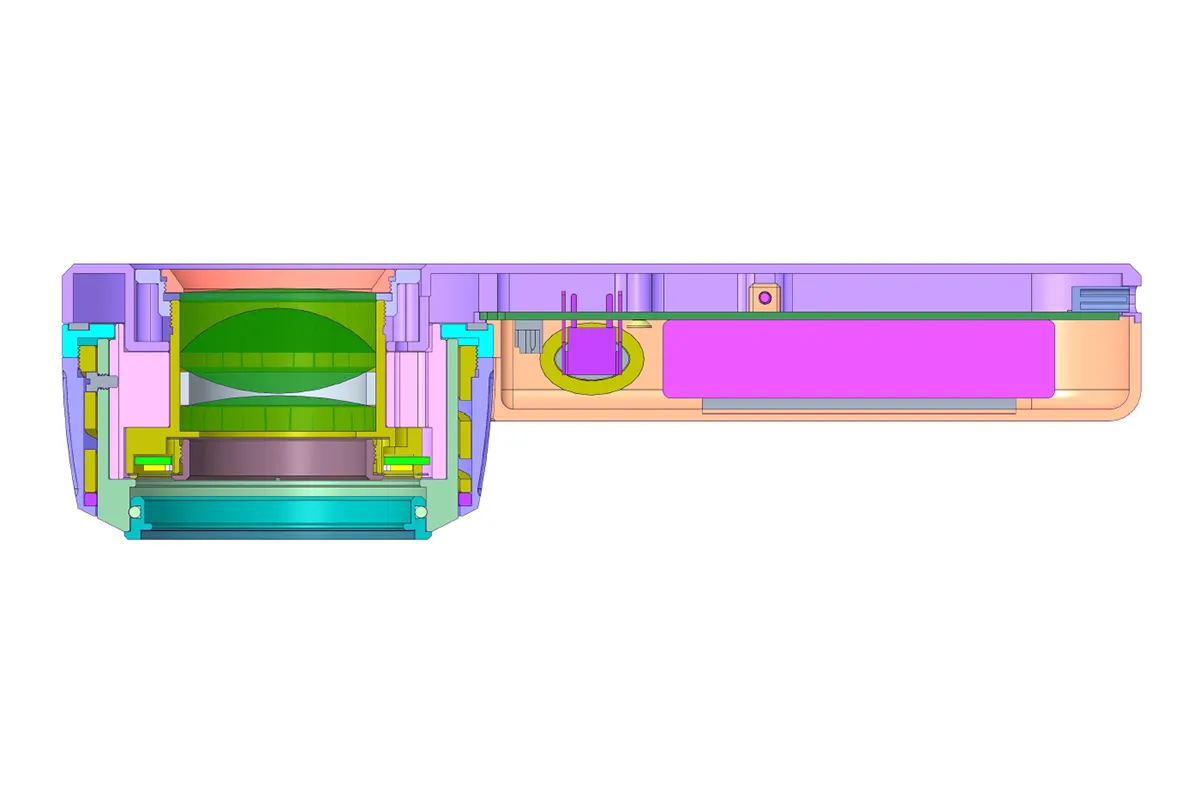
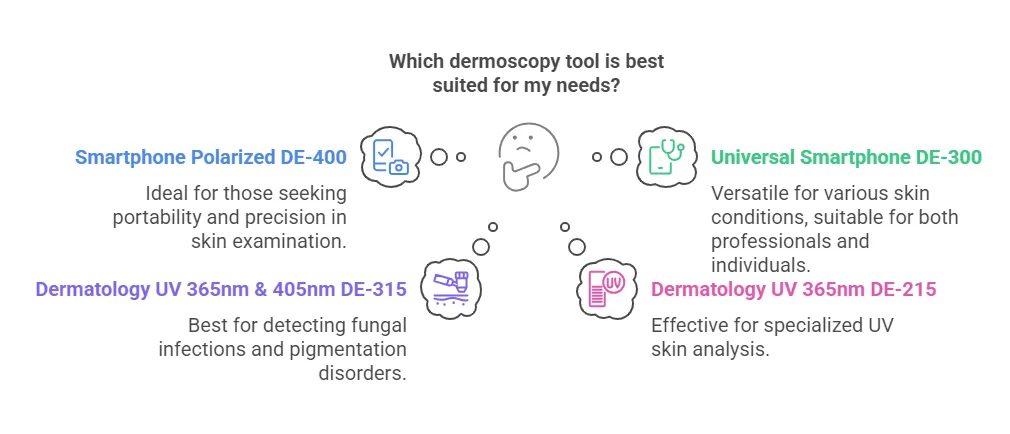
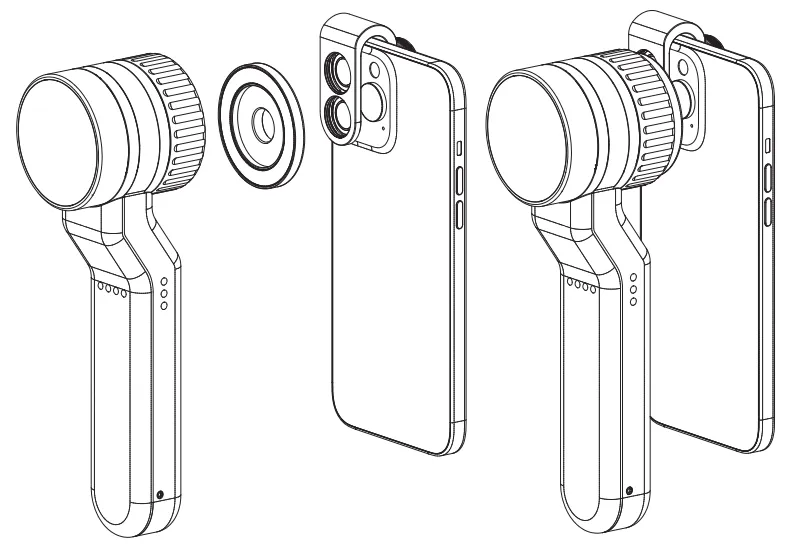
IBOOLO's acral melanoma dermoscopy utilizes advanced polarized light and 20x magnification to non-invasively analyze pigment networks, vascular patterns, and skin texture on palms, soles, and nail beds.
A Practical Guide to Acral Melanoma Dermoscopy: From Basics to Feature Analysis
Acral melanoma, a subtype of melanoma commonly occurring on the palms, soles, or nail beds, has a significant incidence among Asian populations, making early diagnosis critical for improving prognosis. Dermoscopy, a non-invasive diagnostic tool, enhances the identification of characteristic features such as the parallel ridge pattern and irregular pigment distribution, boosting diagnostic accuracy to over 90%. This article provides a comprehensive overview of acral melanoma dermoscopy, covering standard operating procedures, key feature interpretation, and practical clinical techniques to serve as a thorough reference for dermatologists.
What Is Acral Melanoma Dermoscopy?
Acral melanoma dermoscopy involves the use of a specialized optical magnification device to examine the skin’s surface and deeper structures non-invasively. For acral melanoma, which often affects areas like the palms, soles, or nail beds, dermoscopy reveals abnormal pigment patterns, vascular morphology, and textural changes that distinguish benign pigmented lesions from malignant melanoma. Frequently misdiagnosed in its early stages due to subtle presentations, acral melanoma benefits significantly from dermoscopy, which markedly improves early detection rates and serves as a vital clinical aid.
Why Is Dermoscopy Used for Acral Melanoma?
Early acral melanoma may present only as slight pigment irregularities or streaks, often imperceptible to the naked eye. Dermoscopy’s advantages include:
- High-Resolution Imaging: Magnification of 10–100x reveals pigment networks, blue-white veils, and other hallmark structures.
- Reduced Need for Biopsy: Typical patterns like the parallel ridge or irregular diffuse pigmentation allow preliminary differentiation of benign versus malignant lesions.
- Dynamic Monitoring: High-risk lesions, such as subungual melanocytic macules, can be tracked over time for changes.
Studies demonstrate that acral melanoma dermoscopy elevates diagnostic accuracy from 60% to over 90%, making it indispensable for early intervention.
How Does Dermoscopy Work for Acral Melanoma?
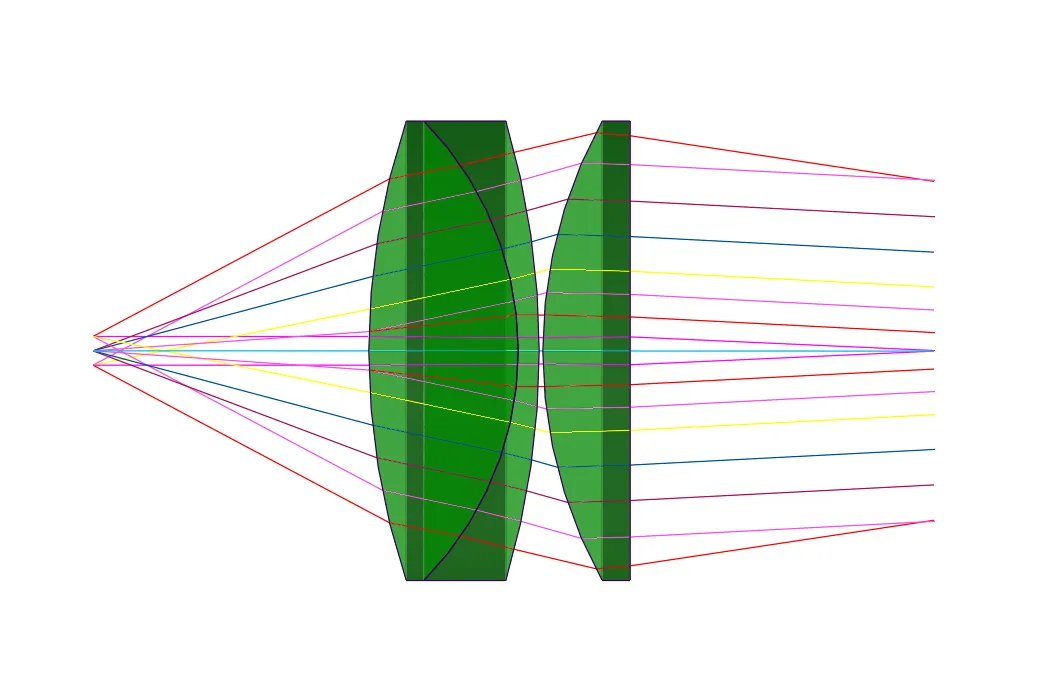
Dermoscopy employs cross-polarized light or immersion oil to eliminate surface reflections, exposing deeper skin features. The unique characteristics of acral sites require specific considerations:
1. Thicker Stratum Corneum: Adjustments in focus or the use of gel enhance light penetration.
2. Pattern Recognition:
- Parallel Ridge Pattern: Pigment along ridge lines, highly suggestive of malignancy.
- Irregular Dots: Disordered brown-black granules.
- Polychromasia: Mixed gray, blue, and red hues.
These features enable precise identification of acral melanoma through dermoscopic analysis.
Can Dermoscopy Detect Early-Stage Acral Melanoma?
Yes, acral melanoma dermoscopy is effective for detecting both in situ (non-invasive) and minimally invasive melanomas:
- In Situ Melanoma: May show subtle pigment network disruptions or dotted vessels.
- Invasive Lesions: Accompanied by blue-white structures, ulceration, or atypical vasculature.
Clinical cases have demonstrated dermoscopy identifying early acral melanoma as small as <3mm, preceding histopathological confirmation, underscoring its sensitivity for early detection.
How to Perform Acral Melanoma Dermoscopy: Step-by-Step Guide
Equipment Preparation:
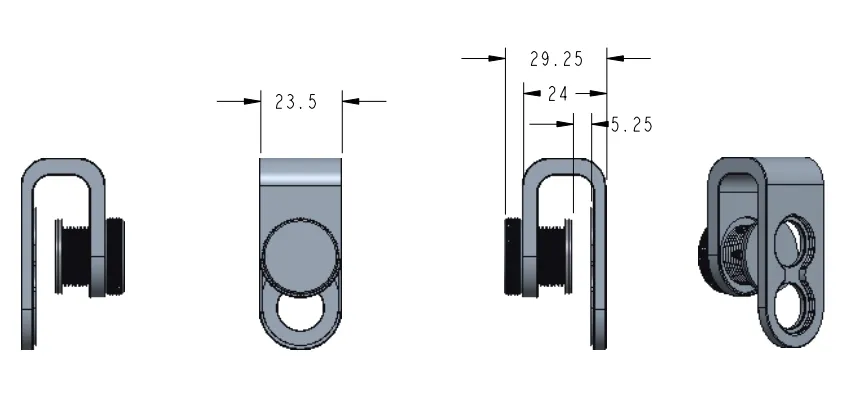
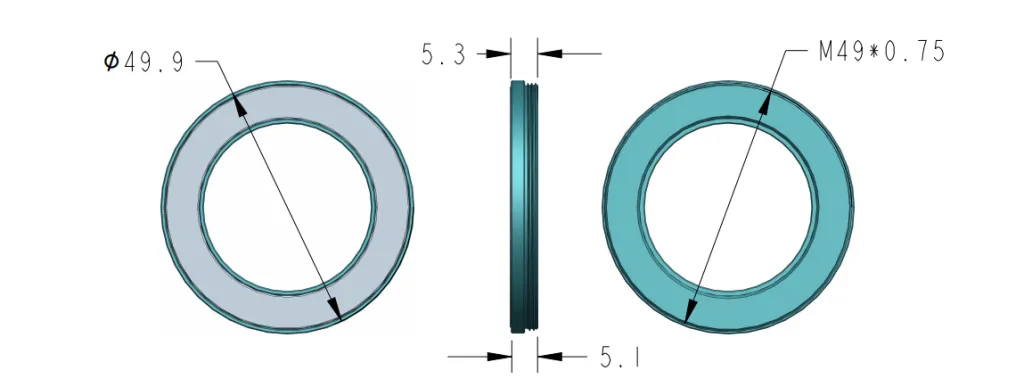
1. Select a polarized or non-polarized dermoscope; use a dedicated adapter for nail bed examination.
2. Clean the skin with alcohol or apply ultrasound gel to reduce glare.
Examination Process:
- Step 1: Assess the lesion’s overall contour and color distribution.
- Step 2: Zoom into specific areas (e.g., edges, center) to evaluate:
- Pigment distribution along ridges or furrows (malignancy indicator).
- Presence of blue-white veils or crystalline structures.
- Step 3: Capture and annotate images of suspicious features for follow-up comparison.
Key Notes:
- For subungual lesions, trim nails and remove keratin debris.
- For plantar lesions, examine after rest to minimize friction-related artifacts.
Does Dermoscopy Replace Biopsy for Acral Melanoma?
While acral melanoma dermoscopy enhances diagnostic precision, biopsy remains the gold standard. Its primary value lies in:
- Screening High-Risk Cases: Reducing unnecessary biopsies for benign lesions.
- Guiding Biopsy Sites: Targeting the most irregular areas to increase histopathological yield.
For instance, findings like “blue-white veil + irregular vessels” prompt immediate excisional biopsy, optimizing diagnostic workflows.
How to Improve Acral Melanoma Dermoscopy: Key Techniques
Magnification Selection:
- 10–20x: Ideal for initial screening and overall pigment assessment.
- 30–50x: For detailed analysis of fine structures (e.g., dotted vessels, blue-white veil).
- 50–100x: Essential for nail matrix evaluation.
Feature Recognition Tips:
1. Adjust lighting angles: Side illumination highlights ridge patterns.
2. Apply pressure: Reduces stratum corneum interference, enhancing vessel visibility.
3. Dynamic observation: Slightly shift the probe to detect pigment variation with angle changes.
Common Pitfalls:
- Over-reliance on single features (e.g., color alone).
- Ignoring clinical history (e.g., lesion growth rate or symptoms).
What Are the Dermoscopic Features of Acral Melanoma?
Key features in acral melanoma dermoscopy include:
- Parallel Ridge Pattern: Pigment along ridge lines (versus furrows in benign lesions), with >90% specificity for malignancy.
- Irregular Diffuse Pigmentation: Mixed brown-black and gray-blue tones with blurred borders.
- Blue-White Structures: Scar-like white areas with blue-gray hues, indicating tumor invasion.
- Polymorphous Vessels: Dotted, hairpin, or spiral vessels, often with hemorrhage.
Comparison Example:
- Benign Nevus: Uniform pigment, parallel furrow pattern.
- Melanoma: Asymmetry, polychromasia, abrupt border interruptions.
How to Differentiate Acral Melanoma from Similar Lesions?
Acral Lentiginous Nevus vs. Melanoma:
Feature:Pigment Distribution、Color Uniformity、Border Clarity。
Acral Lentiginous Nevus:Parallel Furrow Pattern、Even Light Brown、Regular, Gradual。
Acral Melanoma:Parallel Ridge Pattern、Multicolored (Gray, Blue, Red)、Irregular, Abrupt。
Additional Differentiators:
- Traumatic Hemorrhage: History of recent injury, uniform red-black crust under dermoscopy.
- Viral Warts: Red/black dotted vessels without pigment networks.
What’s New in Acral Melanoma Dermoscopy Research?
Recent advances (2023–2024):
1. Confocal Microscopy with Dermoscopy: Boosts in situ detection by 15% with cellular resolution.
2. 3D Dermoscopy Imaging: Reconstructs lesion depth for invasion assessment.
3. Biomarker Visualization: Fluorescent dyes target melanoma-specific proteins (e.g., PRAME).
These innovations enhance detection of “amelanotic” acral melanoma, often missed by traditional dermoscopy.
Can AI Improve Acral Melanoma Dermoscopy Diagnosis?
Current AI Applications:
- Image Analysis Algorithms: Deep learning (e.g., CNN) identifies parallel ridge patterns and irregular vessels, achieving 92% sensitivity (versus 85% for clinicians alone).
- Real-Time Systems: Smartphone-integrated dermoscopes provide instant risk scores (e.g., “High Risk: Biopsy Recommended”).
Limitations:
- Requires high-quality images; thick keratin in nail beds or soles may lead to errors.
- Must complement, not replace, clinical expertise.
Future Prospects: Multimodal AI integrating dermoscopy, pathology, and genetic data.
How to Maintain and Care for Acral Melanoma Dermoscopy Devices
Daily Maintenance:
1. Lens Cleaning: Use lens paper and solution, followed by alcohol wipes post-examination.
2. Light Source Check: Ensure LED brightness is uniform, with no flickering.
3. Calibration: Monthly verification of magnification and color accuracy with a standard card.
Storage: Keep in a dust-proof, dry box (40–60% humidity) to preserve functionality.
Acral melanoma dermoscopy is a cornerstone of modern dermatology, offering a non-invasive, high-accuracy method to detect and monitor this malignancy. By leveraging polarized light to reveal subsurface features like the parallel ridge pattern and irregular pigmentation, dermoscopy empowers clinicians to differentiate acral melanoma from benign mimics effectively. This guide outlines standardized procedures, key diagnostic features, and advanced techniques, supported by evidence of improved early detection and reduced biopsy rates. With ongoing innovations like AI and 3D imaging, acral melanoma dermoscopy continues to evolve, solidifying its role as the dermatologist’s “third eye” for precise, life-saving diagnoses.
Acral melanoma is a special subtype of skin cancer. Late presentation of patients and delayed diagnosis by doctors result in poor prognosis and survival. Despite advances in the understanding of the key features of this disease, early diagnosis of acral melanoma remains challenging. A combination of clinical presentation, dermoscopy, and histologic findings is essential for the diagnosis of acral melanoma.
What is acral melanoma?
Acral melanoma is also known as acral lentiginous melanoma. Acral melanoma is a rare subtype of melanoma. And it usually happens in acral of the body, like palms on the hands, soles of the feet, and under the nails. Unlike other melanomas that is usually caused by over sun exposure and occurs in fair-skinned people . Oppositely, the places include palms, soles and under the nails are not commonly exposed on sunburn. Dark people usually don’t get melanomas. However, acral melanoma is the most common type of melanoma in dark people and it also affect people of all ethnic backgrounds. Hence these these melanomas are found later than other types of melanomas after they invade deeper layers of the skin or metastasize. So it brings more difficult to detect and diagnose the acral melanoma than other skin cancers.

What are the difficulties in diagnosing acral melanoma?
As the acral melanoma is usually found late by patients, there are some difficulties and misunderstandings in the diagnosing acral melanoma as below:
Atypical Presentation: Early acral melanoma lesions are often difficult to diagnose because the pigmentation of the lesions usually follow the skin marking on the palms and soles, resulting in asymmetrical appearance and irregular borders. This similarity with benign melanocytic moles can make early diagnosis difficult.
Misconceptions: There is a misconception that melanoma only happen on the areas exposure in sun. So people always will neglect the changes on other parts of the skin, which causes the delayed diagnosis of acral melanoma.Unfortunately, this will lead to acral melanoma being found at advanced stage and bring a poor treatment effectiveness.
Histopathological complexity: The biopsy and histopathological examination needed to diagnose acral melanoma may be very complexity. Because acral melanoma cells may not present its typical characteristics always. This lead to a potential misdiagnosis.
Advantages of dermoscopy in the diagnosis of acral melanoma
To improve the diagnosis of acral melanoma, it is crucial to use the advanced diagnosis technique dermoscopy. Dermoscopy is a handheld device equipped with a magnifying lens and a light source to allows a enhanced visual for dermatologist to diagnose skin lesions and skin conditions, like acral melanoma and other types of skin cancer. In professional hands, dermatoscope can help to diagnose the very early stage of melanoma by typical structures and patterns which can not visual by naked eyes. In addition, the dermatology is invasive and painless. It not only can avoid the cross infection during examination but also can reduce the unnecessary biopsy and surgery.
Some modern advanced dermoscopes can capture image of lesion or connect to computer software for better analysis.
What are dermoscopic features of acral melanoma?
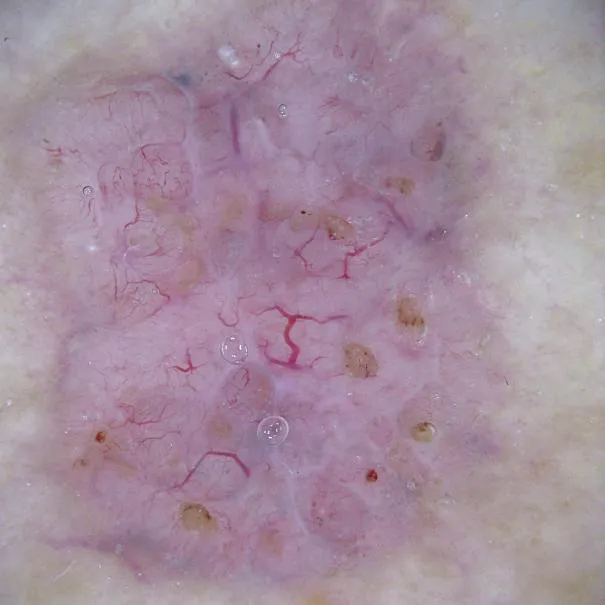
Dermoscopy is an essential tool to help dermatologists diagnose the acral melanoma by providing critical visual clues that differentiate it from benign lesions. There are some key dermoscopic features associated with acral melanoma as below:
Parallel Ridge Pattern: This pattern is characterized by irregular and disrupted pattern that follows the ridges of the skin on the palms and soles.
Irregular Diffuse Pigmentation: Uneven distribution of pigmentation color, often with multiple shades of colors.
Multiple or Mixed Colors: Acral melanoma lesions often present a mix of brown, blue-grey, black, and red colors or multiple colors.
Irregular Dots and Globules: Exhibit of scattered dots and globules of varying size and colors within the lesion.
Atypical Vascular Patterns: Presence of unusual or irregular blood vessels within the lesion.
Asymmetrical and Irregular Border: Acral melanoma with asymmetrical structures and irregular, uneven,notched or blurred borders.
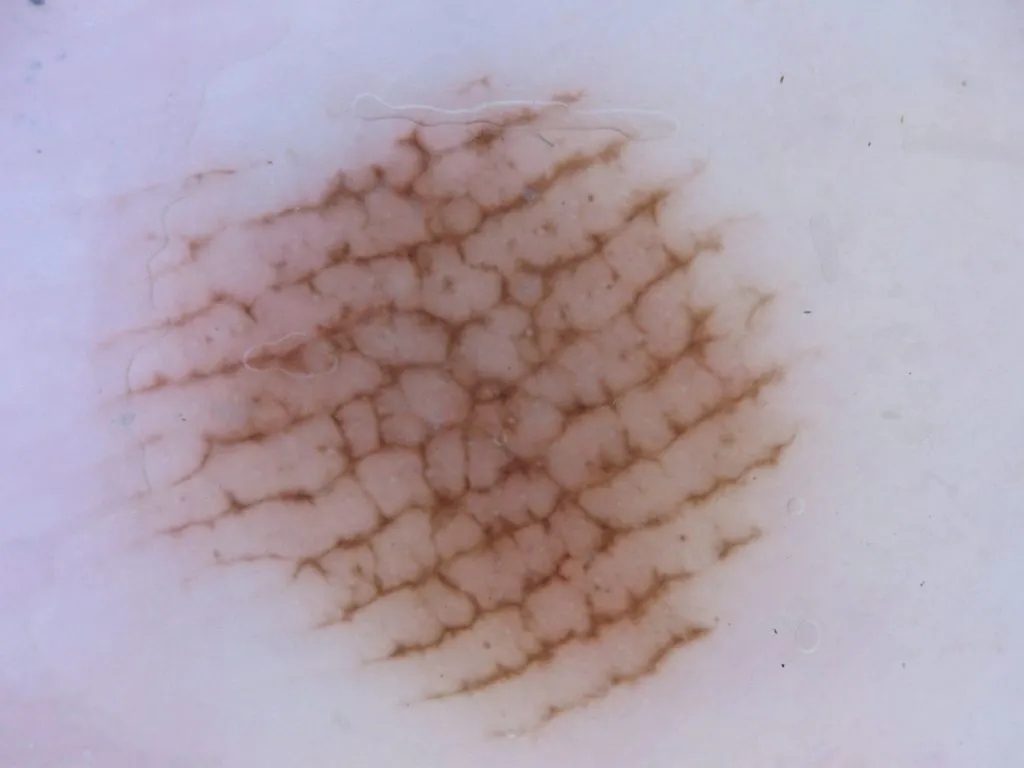
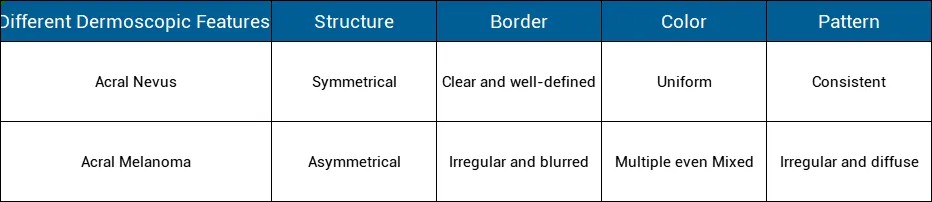
Distinguish the dermoscopic features of similar lesions like acral nevus
Acral nevus (benign melanocytic nevus) and acral melanoma may present similar characteristics. While dermoscopy is a very important and necessary tool tell the differences from them. Here are the key points for distinguishing acral nevus from acral melanoma including:
Exploring the factors affecting the prognosis of acral melanoma
Due to the late inspection and detection of acral melanoma, resulting in a poor prognosis. Except for that, there are some other factors that affect the prognosis of acral melanoma as below:
Feature of the lesion :
Size and Location: If the size of the lesion Larger than 4 mm, and those also located in weight-bearing areas like the soles or under the nails can be more challenging to detect and treat early. This means a potentially worsening prognosis.
Ulceration: Commonly ulcerated lesions are associated with a worse prognosis than the one is not ulcerated.
Thickness: Thickness is the obvious factors which affect the prognosis of acral melanoma. The thicker tumors (greater breslow depth) are often associated with a more worse prognosis.
Stage of the Lesion:
Advanced Stages: Patients diagnosed at advanced stages that means the lesion have invaded into lymph nodes or other parts of the body have a poor prognosis. Advanced stage brings more difficulties in survival rate.
Age and Gender: As reported and analysis, that the older age and the male patients generally tend to have poor prognosis than the young and the female.
Gene mutation :
Commonly gene mutation such as BRAF, KIT, NRAS,and so on, this altered genes can influence prognosis and response to targeted therapies. It causes a poor prognosis of acral melanoma.
Immune System: Especially the patients diagnosed at acral melanoma or other cancers and with low immune system tend to have a worse prognosis than the normal ones.

How to improve the diagnosis of acral melanoma?
As we know that it is difficult to detect and diagnose the acral melanoma especially in its early stage due to its special characteristics. Then how to improve the diagnosis of acral melanoma? There are some methods to improve the diagnosis of acral melanoma including:
People should raise the awareness about the possibility of melanoma in non-sun exposed areas and learn more knowledge about this rare and special skin cancer.
People should do more regular self-examinations by dermoscope, especially of the palms, soles of the feet, and under of nail if there is unusual spots or dots.
People and dermatologists should use dermoscopy, an advanced diagnostic device and techniques to inspect skin situations. Particularly, it is a must to have skin checked by dermoscopy by professional doctors when suspicious lesions are found.
As we can see, early detection are very important to improve the prognosis of acral melanoma. Dermoscope indeed plays a vita role in detecting, diagnosing, monitoring and managing skin lesions and skin cancers like acral melanoma. Dermoscopy is a very valuable and helpful device in the field of dermatology, significantly increasing the ability to inspect and diagnose acral melanoma in early stage. Dermoscopy not only improves patient confidence through early intervention and appropriate treatment schedule, dermoscopy but also reduce the infection during the examination.